With the advent of MIGS, modern glaucoma surgery encompasses a vast array of procedures. While there are several approaches tapping into the conventional outflow pathway such as the iStent and Trabectome, as most glaucoma surgeons know, MIGS procedures that bypass the trabecular meshwork to directly access Schlemm’s canal frequently do not achieve the low intraocular pressures required for patients with advanced disease. Resistance in the downstream outflow pathway has been postulated as a possible explanation.
To achieve very low IOPs and simultaneously avoid bleb-related complications associated with trabeculectomy and conventional posterior tube shunt surgery, many investigators have long sought to develop new surgical approaches to access the suprachoroidal space. Younger ophthalmologists may not know this, but for more than a century and up until the development of the trabeculectomy, the intentional creation of a cyclodialysis cleft was an accepted method for the treatment of recalcitrant glaucoma.
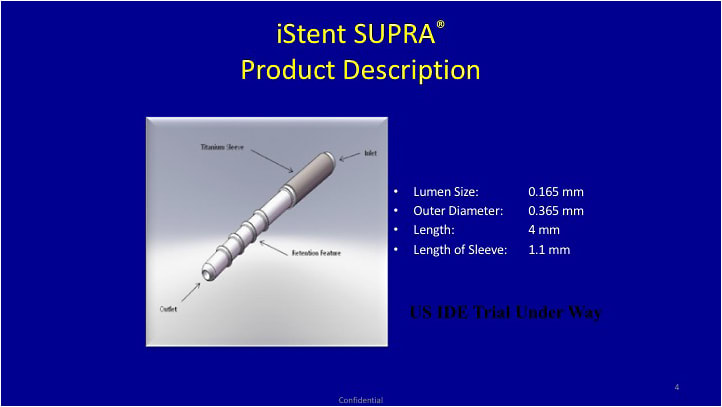
Understandably, that approach was fraught with complications, including hypotony. Newer approaches (albeit not all FDA-approved) utilize flow-restrictive shunts that can be implanted into the suprachoroidal space using either an external approach (STARflo glaucoma implant) or an intracameral approach (SOLX gold shunt, CyPass Micro-Stent and iStent Supra1).
CYPASS
The FDA approved the CyPass Micro-Stent in June 2016. Alcon has begun a measured rollout of the device. Surgeons must undergo the type of training that was required by Glaukos before surgeons were cleared to implant the iStent.
This device is 6.35-mm long, has a diameter of about 0.5 mm and is implanted with an ab interno approach.2 It is slightly curved and attached to a guide wire that aids in implantation during gonioscopic visualization. The device tip is used to bluntly dissect the ciliary body from scleral spur and thereby access the suprachoroidal space. Its retention rings allow it to remain in place while the guide is retracted.


PowerPoint images courtesy Angelo P. Tanna, MD
EFFICACY AND SAFETY
COMPASS was a well-designed clinical trial in which 374 eyes were randomized to cataract surgery and CyPass implantation, while 131 control eyes were randomized to cataract surgery alone. Washed out (unmedicated) baseline IOPs were about 24-25 mm Hg. In a nutshell, CyPass resulted in a modest IOP reduction of about 2 mm Hg more than cataract surgery alone at 24 months. For more detail, 60% of controls versus 77% of CyPass subjects achieved ≥ 20% IOP reduction below baseline at 24 months.
Although this difference was highly statistically significant, favoring CyPass, this study should remind us once again that cataract surgery alone is very effective in lowering IOP. The unmedicated IOP was about 2 mm Hg lower in the CyPass group vs. the control group at 24 months. The clinical trial protocol required a standardized, stepwise approach to re-starting glaucoma medications for patients with IOP > 21 mm Hg. At 24 months, CyPass patients were on 0.2 ± 0.6 medicines vs. 0.6 ± 0.8 for controls (P<0.001).
This surgery is not without risk of complications. Hypotony (2.9%) and cyclodialysis clefts greater than 2 mm circumference (1.9%), were only observed in the CyPass group. Hypotony persisted for less than 30 days in all subjects. Only one case of a persistent cyclodialysis cleft was reported and that patient had an IOP of about 10 mm Hg. In context, the incidence of complications is far lower than would be expected with trabeculectomy or tube shunt.3-5
SUMMARY
The suprachoroidal space holds promise. As these devices are implanted via an ab-interno technique and are not associated with a subconjunctival bleb, conjunctival real estate is preserved and bleb-related complications such as leaks and late infections do not occur. The five-year risk of blebitis was 1.5% in the Collaborative Initial Glaucoma Treatment study; however, trabeculectomy achieves a much lower mean IOP.6
The iStent is also associated with a favorable safety profile compared to trabeculectomy and tube shunt surgery; however, this device can only be used in mild to moderate glaucoma and results in even more modest IOP reduction at 24 months.7 Suprachoroidal implants may represent the intermediate step between a trabecular stent and trabeculectomy or tube shunt surgery.
We must cautiously monitor the incidence of adverse events once these devices are in widespread clinical use. OM
REFERENCES
- Melamed S., Simon B., Goldenfeld M., Simon G. Efficacy and safety of gold micro shunt implantation to the supraciliary space in patients with glaucoma: a pilot study. Arch Ophthalmol. 2009; 127: 264-269.
- Vold S, Ahmed I. Craven E et al., Two year COMPASS trial results: supraciliary microstenting with phacoemulsification in patients with open-angle glaucoma and cataracts. American Academy of Ophthalmology. Article in press.
- Hoeh H., Vold S, Ahmed, I, et al. Initial Clinical Experience With the CyPass Micro-Stent: Safety and Surgical Outcomes of a Novel Supraciliary Microstent. J Glaucoma. 2016; 25:106-112.
- Christakis P, Kalenak J, Zurakowski D, et al. The Ahmed Versus Baerveldt study: one-year treatment outcomes. Ophthalmology. 2011; 118: 2180-2189.
- Gedde S, Herndon L, Brandt J, et al. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 2012;153: 804-814 e1.
- Zahid, S, Musch, D, Niziol L, Lichter P. Risk of endophthalmitis and other long-term complications of trabeculectomy in the Collaborative Initial Glaucoma Treatment Study (CIGTS). Am J Ophthalmol. 2013; 155: 674-680, 680 e1.
- Craven E, Katz L., Wells J, Giamporcaro J. Cataract surgery with trabecular micro-bypass stent implantation in patients with mild-to-moderate open-angle glaucoma and cataract: Two-year follow up. J Cataract Refract Surg. 2012; 38: 1339-1345.









