The advent of intravitreal vascular endothelial growth factor (VEGF) therapy has revolutionized neovascular AMD treatment and remains the standard of care in managing this disease. While patients typically require ongoing injections, the majority can at least achieve preservation, if not improvement, of their visual acuity and quality-of-life measures.
Case in point: In the recently published Comparison of Age-Related Macular Degeneration Treatment trials, which recorded patients’ five-year outcomes with anti-VEGF therapy, 50% of follow-up participants achieved visual acuity of 20/40 or better.1 Furthermore, nearly 10% of patients retained acuity of 20/20. While these outcomes represent a significant improvement over those from natural history studies conducted prior to the anti-VEGF era, significant work remains, as evidenced by the nearly 20% of individuals with a visual acuity of 20/200 or worse after five years.1
But, to reduce the overall treatment burden on retinal specialists and patients from serial anti-VEGF injections, researchers are investigating numerous targeted therapies that could improve visual outcomes for patients better than current options and also decrease the overall costs of treatment on the health-care system. One strategy that has generated a significant amount of interest within the medical community is gene therapy and its potential for long-term sustained production and release of VEGF in vivo.
The objective of gene therapy is to provide continual expression of a protein(s) of interest involved in the pathogenesis of a relevant disease process for a sustained therapeutic benefit. The desired genetic information encoding a protein(s) of interest is carried via viral vector into the target cells. Successfully transduced vectors then use the host cell’s machinery to express the particular protein(s).
Gene therapy for retinal degenerative diseases is receiving significant research and developmental focus, with several therapies progressing through human clinical trials. In the world of AMD, the two main categories of vectors being investigated are integrating vectors and nonintegrating vectors. Integrating vectors (i.e. lentiviral vectors) insert themselves into the recipient’s genome, whereas nonintegrating vectors (i.e. adeno-associated virus [AAV]) usually form an extrachromosomal genetic element. This article describes the gene therapies currently progressing through clinical trials.
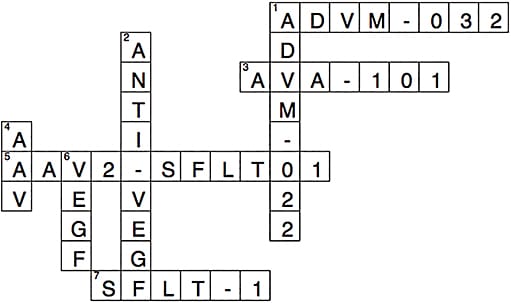
INTRAVITREAL AAV2-SFLT01
The secreted extracellular domain of sFlt-1 is a soluble isoform of the VEGF receptor 1, and a naturally occurring protein antagonist of VEGF. Adeno-associated virus type 2 (AAV2)-sFLT01 (Genzyme) is a replication-deficient, adenovirus-associated viral vector with a plasmid that expresses a portion of the sFlt-1 VEGF receptor termed sFLT01.2 sFLT01 encodes domain 2 of sFlt-1 linked to a human immunoglobulin G1 heavy chain Fc fragment. After the viral vector is injected intravitreally, it transfects native cells to produce the modified protein. This has been well-tolerated in monkeys.3 Intravitreal AAV2-sFLT01 is being studied in phase 1 clinical trials in human subjects with neovascular AMD.4
SUBRETINAL AVA-101 AND INTRAVITREAL ADVM-022, ADVM-032
Like Genzyme’s lead candidate, AAV2-sFLT01, Adverum Biotechnologies (formerly Avalanche Biotechnologies) developed a similar replication-deficient AAV2 vector containing the sFLT-1 plasmid (AVA-101). However, in contrast to the intravitreal approach, AVA-101 was to be injected into the subretinal space, requiring concurrent vitrectomy surgery.
Initial phase 1 studies demonstrated that AVA-101 was well tolerated in the six study participants with no significant drug-related safety concerns.5 In late 2015, top-line results from a phase 2a study involving 32 patients with advanced AMD became available.6 Patients were randomized into the AVA-101 treatment group (n=21) or control (n=11). Subjects in both arms received two initial ranibizumab (Lucentis, Genentech) injections at day 0 and week 4, followed by ranibizumab rescue therapy as early as week 8, according to prespecified criteria. Twenty-nine of 32 subjects received prior anti-VEGF therapy (average of 10 prior injections).
The reported data met the primary endpoints in terms of ophthalmic and systemic safety measures; however, secondary endpoints assessing functional and anatomic outcomes were not as clear. In terms of visual improvement, the mean change from baseline showed a difference of 11.5 letters between the treatment (2.2 letters gained) and the ranibizumab control (9.3 letters lost) groups. The degree of vision loss in the control group was uncharacteristic but attributed to the refractory nature of disease displayed by many of the participants who received extensive previous anti-VEGF treatment prior to enrollment. A significant number of AVA-101 treated subjects (43%) improved or maintained stable vision with two or fewer rescue injections, compared with subjects in the control group (9%). With regard to anatomic changes, the treatment group demonstrated a mean increase of 25 μm over baseline in central retinal thickness measurements on OCT compared to a mean decrease of 56 μm in the control group.6 After further analysis of these results, the company announced in late 2015 that it would no longer initiate a phase 2b trial on AVA-101.
Since then, Adverum has since shifted its focus toward developing its next-generation candidates: ADVM-022 (AAV.7m8-aflibercept) and ADVM-032 (AAV.7m8-ranibizumab). In contrast to AVA-101, which used a wild type AAV2 vector, ADVM-022 and ADVM-032 each employ a novel vector that has been optimized for intravitreal injection rather than the more invasive surgical subretinal delivery. Adverum presented preclinical efficacy data on both agents in a laser-induced choroidal neovascularization (CNV) nonhuman primate model at The Retina Society 2016 Annual Meeting.7 A single intravitreal administration of either ADVM-022 or ADVM-032 demonstrated comparable efficacy to conventional intravitreal anti-VEGF therapy for inducing regression of CNV lesions. Additionally, pharmacokinetic studies of the vitreous and retinal tissue showed durable anti-VEGF protein expression with therapeutic protein levels achieved at least 20 weeks after the injection while maintaining a favorable safety profile (out to 26 weeks). The company plans to continue development of both programs with human studies in the future.
SUBRETINAL RETINOSTAT
RetinoStat (Oxford BioMedica) is an equine infectious anemia viral lentiviral vector expressing the genes of two naturally occurring inhibitors of angiogenesis: endostatin and angiostatin. Subretinal injection of RetinoStat into monkey and rabbit models has shown that this product is capable of persistent, localized gene expression.8,9 On the basis of pre-clinical data, it is anticipated that RetinoStat may require only a single administration if proven safe and effective in human trials.
A phase 1 clinical trial (GEM) enrolling 21 patients with advanced neovascular AMD was recently completed. These participants received escalating doses of subretinally injected RetinoStat.10 The study met the primary endpoints of safety and tolerability at six months postsurgical transfection.11 In addition, patients showed signs of clinical benefit, with stabilization of vision and an anatomic reduction in vascular leakage. Successful retinal transduction was demonstrated by a substantial increase in expression and secretion of endostatin and angiostatin proteins, as measured in the anterior chamber of the study eyes.11 Longer-term protein expression has been sustained for up to one year post-treatment, and preliminary data show a dose response, with the escalation to higher dose levels yielding a proportional increase in average protein expression.11
CONCLUSION
Research evaluating the potential of gene therapy in treating AMD as well as other retinal degenerative conditions has progressed significantly over the past decade. While not without its setbacks, gene therapy research, with the growing body of preclinical and early clinical data, continues to support the safety and efficacy of this exciting treatment.
The significant potential benefits of sustained pharmacologic treatment with a single administration continue to motivate the development of these early stage programs into more advanced phase clinical trials in the coming years. OM
REFERENCES
- Comparison of Age-related Macular Degeneration Treatment Trials (CATT) Research Group, Maguire MG, Martin DF, et al. Five-year Outcomes with Anti–Vascular Endothelial Growth Factor Treatment of Neovascular Age-Related Macular Degeneration: The Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology. 2016;8:1751-1761.
- Pechan P, Rubin H, Lukason M, et al. Novel anti-VEGF chimeric molecules delivered by AAV vectors for inhibition of retinal neovascularization. Gene Ther. 2009;16:10-16.
- MacLachlan TK, Lukason M, Collins M, et al. Preclinical Safety Evaluation of AAV2-sFLT01 — A Gene Therapy for Age-related Macular Degeneration. Mol Ther. 2011;19:326-334.
- Heier JS. Preliminary results of phase 1 study with AAV2-sFLT01 as gene therapy for treatment of exudative AMD: one-year results of phase 1 clinical trial with rAAV.sFLT-1. The Retina Society 2014 Annual Meeting. Sept. 11-14, 2014. Philadelphia, Pennsylvania.
- Heier, JS. Gene therapy for exudative AMD: one-year results of phase 1 clinical trial with rAAV.sFLT-1. American Society of Retinal Specialists (ASRS). Aug. 9-13, 2014. San Diego, California.
- Avalanche Biotechnologies, Inc. Announces Positive Top-Line Phase 2a Results for AVA-101 in Wet Age-Related Macular Degeneration. Adverum Biotechnologies. Http://tinyurl.com/gvh4bjl .
- Blumenkranz M. Surveying the past and charting a path forward for the successful treatment of macular degeneration with gene therapy techniques. The Retina Society 2016 Annual Meeting. Sept. 14-17, 2016. San Diego, California.
- Balaggan KS, Binley K, Esapa M, et al. EIAV vector-mediated delivery of endostatin or angiostatin inhibits angiogenesis and vascular hyperpermeability in experimental CNV. Gene Ther. 2006;13:1153-1165.
- Binley K, Widdowson PS, Kelleher M, et al. Safety and biodistribution of an equine infectious anemia virus-based gene therapy, Retinostat, for age-related macular degeneration. Hum Gene Ther. 2012;23:980-991.
- Phase I Dose Escalation Safety Study of RetinoStat in Advanced Age-Related Macular Degeneration (AMD) (GEM). ClinicalTrials.gov . https://clinicaltrials.gov/ct2/show/NCT01301443 . Accessed March 1, 2017.
- OXB-201 (RetinoStat): A novel gene-based treatment for neovascular “wet” age-related macular degeneration. Oxford Biomedica. http://www.oxfordbiomedica.co.uk/oxb-201-retinostat-r/ . Accessed March 1, 2017.









