Ladas IOL formula continues evolving
And increasing in accuracy, as surgeons feed more data into this fusion of sweet spots of other IOL formulae.
By Uday Devgan, MD, FACS, FRCS
More different IOL formulae exist now than ever before. Recently the Barrett formula, Olsen formula, and the Hill-RBF method have received press for their takes on IOL calculations. But what about the fourth-generation multivariable Holladay 2 and Haigis formulae? And does that mean we should shy away from the third-generation Holladay 1, Hoffer Q, and SRK/T? Do we still need to use the Wang-Koch axial length adjustment for longer myopic eyes? Do we still need to be careful with using the SRK/T in eyes with unusual keratometry? Too many questions!
A busy cataract surgeon needs lots of time to develop decision trees and what-if scenarios per patient listed in the day’s surgical line-up — it is not unheard of for those trees and scenarios to begin to resemble each other. This is precisely where the Ladas super formula comes into play – this amalgamation of many different methods is plotted into 3-dimensional space and automatically does the most precise calculation for each eye. The goal of this formula, introduced a year ago, has always been to give the best refractive outcome in any situation while providing surgeons with an individualized yet dynamic approach that will continuously evolve to become more and more accurate.
Since first publishing the Ladas formula, and then the website, early this year, we have had hundreds of surgeons serve as beta testers for the super formula via www.IOLcalc.com. These surgeons have entered thousands of eyes for IOL calculations. These pre-op and postop data showed some important results, particularly in regards to small eyes with short axial lengths. Small eyes are notoriously difficult to calculate since even a small change in the effective lens position can alter the lens power calculation. The super formula evaluated results of eyes with axial lengths under 22 mm and found that an adjustment to the 3-dimensional super surface was needed. This part of the curve was adjusted with actual patient data so that the entire super surface evolved to become even more accurate.
Users’ reactions
Surgeons visiting the website have noted that using the formula has saved them many hours from creating trees, since this task can be delegated to technicians, as the website does all the decision making. There is also no need for a surgeon to account for unusual eyes, do adjustments for certain axial lengths, or look at “what-if” scenarios. This new formula comes up with a single answer for any IOL calculation query. If the surgeon can save 10 minutes in the planning of each cataract surgery, this adds up to one or two hours per week for an average surgeon and even more for busier ones. Over the course of the year this can save 100 hours or more of surgeon time, and that has real value when balancing a busy practice with home life.
How we got here
Less than a year ago, JAMA Ophthalmology published “A 3-D ‘Super Surface’ Combining Modern Intraocular Lens Formulas to Generate a ‘Super Formula’ and Maximize Accuracy.”1 It was and continues to be a different way to think about IOL accuracy that hadn’t been achieved before. The Ladas uses the sweet-spots of the best available formulae and then makes a cohesive 3-dimensional Super surface.
As Michael Hee, MD, stated in his invited commentary on the article, the super formula “formalized” the approach to use of many formulae.2 Any previously described, current formula and future formulae or methods can be included in the Ladas super surface, which will continually evolve with time.
The formula’s creators also believe that this approach will be helpful to surgeons. Said one anonymous reviewer to our original publication: “What a profound theoretical approach to the time consuming and difficult problem of choosing the best formula for extremes of keratometry, axial length and expected lens position. I hope to use this as soon as possible on all my IOL calculations.”
So with this “formalized” approach, we did a few things. First, we started an interface that was immediately available to any ophthalmologist who was interested in using our formula. We then received input from hundreds of ophthalmologists who have registered as initial beta testers. Very constructive changes were suggested and implemented to the platform.
We sought to make the interface as user friendly and inclusive as possible; see for yourself — the current interface is Figure 1.
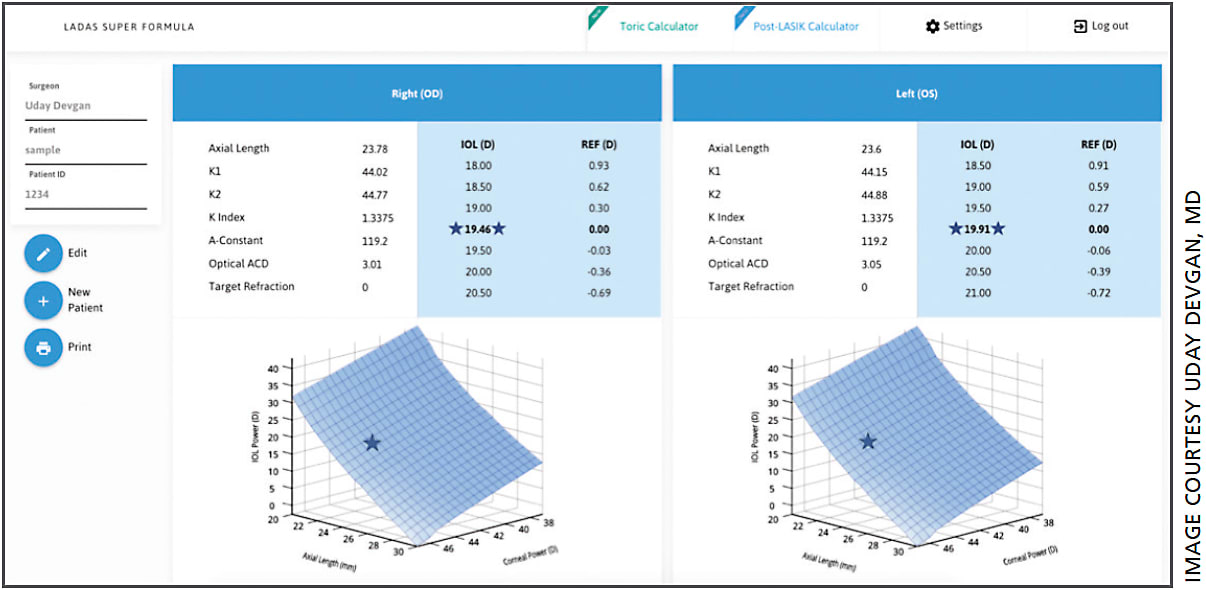
FIGURE 1. INTERFACE ON IOLCALC.COM
The online interface at IOLcalc.com shows both eyes calculated and plotted side by side. With the input data the Ladas super formula automatically performs the best calculation for those specific eyes without the need for the user to do any adjustments such as for long axial lengths.
The interface allows simultaneous calculation and plotting of both eyes. Input-data at this point includes the keratometry, axial length, corneal index and anterior chamber depth. The lens A-constant and desired postop refraction are then selected and the optimized calculations are then performed. The inclusion of the three-dimensional graph is key for a surgeon to know instantly if his patient has typical or unusual eyes. A dedicated toric calculator and a post-LASIK calculator are also included.
How people are using it
Irene Kuo, MD, of the Wilmer Eye Institute, Johns Hopkins University, has utilized the formula on some of her difficult cases such as very long and myopic eyes where care must be taken to avoid a postoperative refractive surprise. Because she used the formula, she did not have to decide or remember when and how to use the Koch axial adjustment or if it would require a negatively powered IOL with different lens geometry.
While allowing use of this methodology as soon as possible was important, we also wanted a more passive approach. We organized a group of high volume surgeons to analyze and track outcomes. At this point, we have downloaded tens of thousands of biometry scans. One way that we can represent this is demonstrated in Figure 2. We call it the “Manhattan graph.”
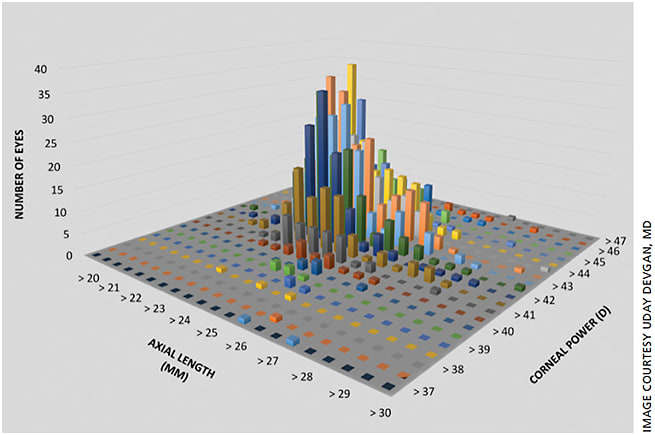
FIGURE 2. This “Manhattan graph” represents the data set of eyes calculated for one surgeon. We can see that while most eyes have an average keratometry and axial length, there are also outliers.
We can visualize and track specific regions of the surface. Figure 3 shows a graph of a representative set of IOLMaster (Zeiss) downloads from a major user group. We can take the data from many surgeons and pool them together to look at specific regions of the super surface and to test hypotheses such as the influence of other parameters on calculations. We can even compare them with any other existing formula.
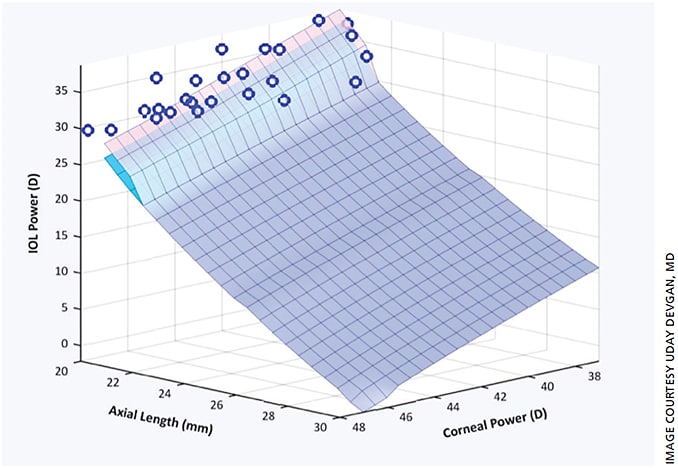
FIGURE 3. A REPRESENTATIVE “LEARNED” FORMULA FOR A SMALL SUBSET OF DATA
The original Ladas super surface has evolved to enhance accuracy in small eyes with short axial lengths. The blue circles represent data points of actual postop results that allow us to alter the optimized Super Surface (lavender/pink) compared with the original (turquoise blue, which is mostly overlapped by the new surface).
Another user is Jonathan Solomon, MD, from Solomon Eye Associates, who has supplied meticulous outcome data on thousands of eyes. “I am happy to help with this project. They have made it very easy to contribute my data and I’m impressed with the analysis.”
Future
It has been repeatedly stated that the key to formula accuracy is optimization and the Ladas formula and surface will continue to evolve and improve. Even if you feel that there is a new single formula that is perfect for all eyes, you can choose to have all your individual data represented in the Super surface that is customized to you. The more data that are imputed, the more precise your measurements will be.
John Ladas, MD, PhD, has been collaborating with Georgetown mathematician Paul Kainen, PhD, on the evolution of the formula to achieve various nonlinear optimizations. This process involves computerized adaptive “machine learning” and “neural networks” to further improve this formula over time.
For instance, we can locate and track records of individual eyes that are outliers and use sophisticated algorithms that determine the important variables to use and enhance the formula. Jack Holladay, MD, who described different types of eyes based on anterior segment size correlated to axial length, was brilliant in his intuit capacity to understand this.
Everyday people
However, not everyone is a math genius like Dr. Holladay, Douglas Koch, MD, or any of the other thought leaders who developed IOLs calculations, so leaning on today’s high-speed computers to arrive at the necessary algorithms is perfectly okay and in fact can be better than any single calculation.
Again, corneal power and axial length, the two axes on our graph, are the two most important variables to calculate any IOL power. We agree that there are other variables (or dimensions) that may or may not make a difference, but to visualize we chose the most important. Yes, the Ladas super formula can also take into account white-to-white, lens thickness, refraction, age, or any other variable related to the eye in order to hone the IOL calculation results.
Conclusion
Because this unique method of 3-dimensional graphing can adapt and evolve to produce more accurate results no matter what new technology comes along, ophthalmologists can now totally focus on surgery and the best results for their patients and leave the mathematics to the Ladas super formula.
Or, as Tamela Martin, MD, put it:
Hi there — I know you are overwhelmed with emails & comments. I really wanted to thank you for your “Einstein quality innovative formula!”
You guys have made my life so much better. Thank you a million times over! OM
REFERENCE
1. Ladas JG, Siddiqui AA, Devgan U, et al. A 3-D ‘Super surface’ Combining Modern Intraocular Lens Formulas to Generate a ‘Super formula’ and Maximize Accuracy. JAMA Ophthalmol. 2015;133:1431-1436.
About the Author | |

| Uday Devgan, MD, FACS, FRCS is in private practice at Devgan Eye Surgery in Los Angeles, a partner at Specialty Surgical Center in Beverly Hills, Chief of Ophthalmology at Olive View UCLA Medical Center, and clinical professor of Ophthalmology at the Jules Stein Eye Institute at the UCLA School of Medicine. He can be reached at www.DevganEye.com, devgan@gmail.com or 1-800-337-1969.
|








