Alternatives to excimer for thin cornea patients
How technology is addressing the limits of the residual stromal bed.
By Amin Ashrafzadeh, MD
Since the early days of LASIK, ophthalmic surgeons have honed their understanding of the technology and the eye-care advancements it’s made possible.
Along with its opportunities, LASIK presents some drawbacks. Researchers soon established that LASIK could carry serious consequences for some patients, such as ectasia for those with thin corneas and with high myopia, those of young age and those with abnormal topographies.1
This article reviews what the discipline has learned about LASIK surgery for patients with thin corneas and their options for visual corrections both currently and in the near future.
ECTASIA PREVENTION METHODS
Stromal bed size
After an uptick in ectasia cases following excimer laser corneal refractive surgery,2 ophthalmologists self-imposed a 250-µm standard residual stromal bed minimum.3,4 According to a survey from ASCRS, 37.7% of surgeons set their personal limits to a more conservative 300 µm.4 However, I wonder if these numbers were reached arbitrarily. I have cared for several post-LASIK ectasia patients who had residual stromal beds of greater than 300 µm. On the other hand, I know some surgeons who have patients with residual stromal beds of well less than 250 µm who have remained stable for over a decade. This is strictly anecdotal, but it raises the question: Is a 250-µm residual stromal bed really a “magic number” that cannot be violated? Perhaps these views will change as improved technology gives us a better picture of corneal health and stability.
Collagen cross-linking
Collagen cross-linking is still under study in the United States. Many of our colleagues are performing this procedure under clinical trial and investigational uses. The data still needs to be fully explored, but, today, a patient such as the one in Figures 1 and 2 may be offered collagen cross linking to stabilize his refraction from further deterioration and potentially reverse some of the ectasia. In 1999 no such option existed. Additionally, some are advocating that options such as combined collagen crosslinking with PRK ablation may be an option.
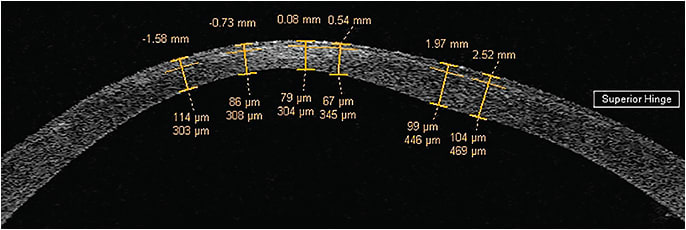
Figure 1. The exacerbated post-LASIK ectasia of a patient having undergone LASIK with two sequential enhancements without success. Residual stromal bed was however preserved above 300 µm.
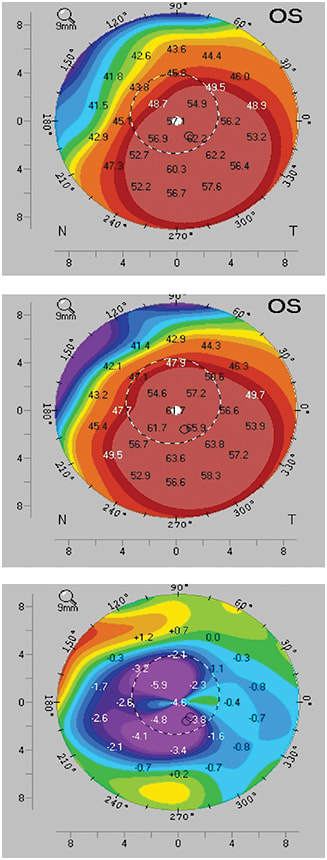
Figure 2. A male patient with keratoconus (from top to bottom): six months after epi-off corneal collagen cross-linking, preoperatively, and his difference map.
COURTESY: WILLIAM TRATTLER, MD
Residual stromal bed minimum
In a survey conducted by ASCRS, surgeons reveal the minimum predicted or true measured residual stromal bed thickness they require for corneal surgery. Most said 250 µm,4 but that number isn’t a hard and fast rule.
200 µm

225 µm

250 µm

275 µm

300 µm

325 µm

350 µm

Hybrid contact lenses
Another avenue to consider is the standards in vision correction: glasses and contacts. Whereas in 1999 patients similar to the one in Figures 1 and 2 had only a choice of a hard or a soft contact lens, a number of much better designed, more comfortable hybrid contact lenses are now readily available.
Not only do these hybrid lenses provide improved comfort, they also provide the excellent optics of a hard contact lens. Many practices provide these special sets of contact lenses.
SURICAL OPTIONS
Phakic IOLs
Surgical alternatives to excimer include IOL options that have either replaced or been adjunct to the excimer laser procedures. Whereas our current excimer platforms can correct to -14.0 D of myopia, treatments above 10 diopters are not ideal, and the phakic IOLs are able to more safely expand our range of treatment for myopia up to -20 D, while preserving the natural lenticular accommodation.
I had a 52-year-old patient with -14 D of myopia and corneal thickness of 520 microns, which limited her capacity to have excimer treatment. She was a successful monovision contact lens user, who progressively became more uncomfortable with her soft contact lenses. She opted for monovision with phakic IOLs rather than multifocal IOLs, given the potential dysphotopsias and the contrast loss. Another factor in her decision was the capacity to preserve her options for future developments.
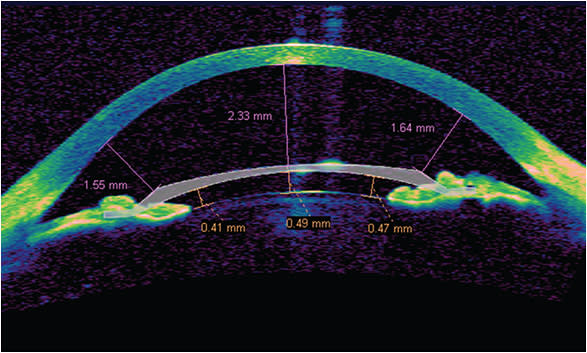
Figure 3. A combined case of IntraLase LASIK and Verisyse lens for correction of high myopia with astigmatism.
Refractive lens exchange
With IOLs, we now have much fewer limitations. Whereas high hyperopia would not be considered ideal on any excimer platform, treating someone at age 50, for example with +7.0 D of hyperopia, refractive lens exchange might be most ideal.
What if the same 50-year-old +7.0 D hyperope also had 3.0 D of astigmatism and he really wants a presbyopic correcting IOL? A combined refractive lens exchange and a later LASIK surgery would address all of the patient’s needs. Performing procedures such as Visian ICL, artisan type iris fixated phakic IOLs, or refractive lens exchange, have their own sets of benefits and concerns.
Surgical evaluations
Before performing any surgery on patients with thin corneas, ophthalmologists should first determine whether the cornea is otherwise normal. Preoperative surgical evaluation can be determined using corneal topography (Figure 2) optical coherence tomography, Scheimpflug imaging or slit imaging.
New procedure avoids flap
A new format of laser vision correction uses the femtosecond laser to create a lenticule in the mid-stroma, which is then extracted through a small incision. The laser first passes a cut in the deeper/posterior stroma and then makes a second pass anteriorly through the stroma. The tissue that is sandwiched between the two passes (the lenticule) is then removed through a small side cut.
Perhaps this new format of laser vision correction will alter our current ideas and concepts in corneal health, stability and safety. Current day LASIK surgery involves creation of a flap in the anterior stroma. Data suggest that more corneal tensile strength resides in the anterior 40% of the cornea than the posterior 60% of the cornea.5 This, in effect, means that when we make a flap, this flap disrupts a significant portion of the cornea where the greatest tensile strength resides.
Perhaps by not disrupting the anterior stroma, but directly removing corneal tissue in the mid or posterior stromal tissue, and even violating the current standard of 250 µm of residual stromal bed, we can still retain similar corneal strength to our current day LASIK.6
Should this technology (ReLEx SMILE, under development by Carl Zeiss Meditec) improve safety, perhaps we can treat patients whose corneas are much thinner and who have a greater treatment profile than we can today.
Armamentarium of treatment
Our increased comfort with phakic IOLs and refractive lens exchange procedures has increased our armamentarium of treatments that best suit each individual’s desires and any anatomical considerations. Over the next few years, I anticipate learning more about collagen cross-linking and other procedures in the pipeline to help accommodate an even greater range of patients. OM
REFERENCES
1. Tatar MG, Kantarci FA, Yildirim A. Risk Factors in Post-LASIK Corneal Ectasia. J Ophthalmology;2014: Published 3 June 2014. Accessed 17 November 2014.
2. Woodward M, Randleman JB, Russell, R, et al. Visual rehabilitation and outcomes for ectasia after corneal refractive surgery. J Cataract Refract Surg. 2005;31:2035–2038.
3. Randleman JB, Russell B, Ward MA, et al. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110:267-275.
4. Leaming DV, Duffey RJ. Leaming. 2011 Survey of American Society of Cataract and Refractive Surgery Members. http://www.analeyz.com/AnaleyzASCRS2011.htm. Accessed Nov. 25, 2014.
5. Randleman JB, Dawson DG, Grossniklaus HE, et al. Depth-dependent cohesive tensile strength in human donor corneas: implications for refractive surgery. J Refract Surg. 2008;24:S85-S89.
6. Reinstein DZ, Archer TJ, Randleman JB. Mathematical model to compare the relative tensile strength of the cornea after PRK, LASIK, and small incision lenticule extraction. J Refract Surg. 2013;29:454-60.doi:10.3928/1081597X-20130617-03.
About the Author | |

| Amin Ashrafzadeh, MD is a cataract, corneal and refractive surgeon in private practice at Modesto Eye Center, Modesto, Calif.
|








