Ocular Cicatricial Pemphigoid
Accurate diagnosis, staging and systemic treatment.
BY C. STEPHEN FOSTER, MD, FACR, FACS
NOT EVERYTHING THAT LOOKS LIKE OCULAR CICATRICIAL PEMPHIGOID (OCP) IS OCP. In addition to OCP, chronic cicatrizing conjunctivitis may occur as a result of various disorders, some of which lead to irrevocable blindness if not correctly diagnosed and treated. Examples of such diseases include Stevens-Johnson syndrome, epidemic keratoconjunctivitis (EKC), Lyell’s disease, rosacea, eczema, scleroderma, lichen planus, trachoma, ligneous conjunctivitis, Sjögren’s syndrome, linear IgA disease, pemphigus vulgari and sarcoidosis.
This is why immunohistochemical analysis of conjunctival biopsy is the standard of care for a definitive diagnosis of OCP before starting immunomodulatory therapy. Commencing such therapy in a person with eczema, rosacea, or scleroderma, for example, would be ill advised.
The key to staying out of trouble for patients with ocular inflammatory disease of any sort, any time, is a detailed history with a careful review of systems, detailed examination of skin and mucous membranes including these tests:



The best biopsy results come from snap-frozen conjunctiva. Do not use formalin. Put the biopsy in saline until you can get it to an immunopathologist who will freeze it, put it in optimum cutting temperature compound, make frozen sections and perform the immunoprobing.
OCP is a systemic disease. Like many autoimmune diseases, it has a documentable genetic predisposition, called the DQ beta-1 star 0301.
Its manifestations can only be ocular, but more commonly, patients have other symptoms. The disease is potentially fatal if it involves the esophagus, which is why it’s crucial to query these patients about episodic dysphagia, or choking while trying to swallow. If that emerges from the history, then they need esophagoscopy.
Patients who are genetically predisposed to develop this disease have an autoimmune response that results in the production of an autoantibody. The autoantibody recognizes a particular peptide, namely beta-4 peptide of alpha 6 beta 4 integrin, an adhesion molecule in hemidesmosomes in conjunctival basal epithelium. All local attempts to control OCP will fail because of its systemic nature.
The disease has four stages:




We see a network of subepithelial fibrosis at Stage 1, which then contracts and causes fornix foreshortening at Stage 2. And with the first appearance of symblepharon, the patient is at Stage 3. Stage 4 is the end result. Nothing can be done for Stage 4 OCP. We want to treat this very early — at Stage 1 if possible — but we usually don’t see patients until at least Stage 2.
Lou Wilson, Marilyn Ekins, (of Emory University) and I published the first work about treating OCP systemically, namely with cyclophosphamide. In 1986, I reported on two randomized controlled trials of drug therapy for OCP, in my American Ophthalmological Society thesis. By far the most effective recipe for treating this disease, intravenous immunoglobulin (IVIG) and rituximab (Rituxan, Genentech), is also the most aggravating logistically and financially. I only turn to it first if I’m inheriting a patient in an advanced stage of the disease.
In patients with biopsy-proven OCP that is active and documented to be progressive, I generally start, if the disease is not rapidly progressing, with methotrexate, mycophenolate mofetil (CellCept, Genentech) or azathioprine first. Methotrexate is safer than diaminodiphenylsulfone (Dapsone). It’s so amazingly easy to use — once weekly by mouth, and they’re done. It takes care of about 70% of instances of Stage 1 or Stage 2 OCP. Mycophenolate mofetil is also good, but it’s more tedious than methotrexate because it’s taken twice a day on an empty stomach (no food an hour before or 2 hours after). Azathioprine has a good track record as well.
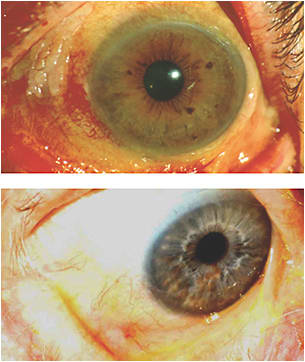
FIGURE 1. This patient with OCP was treated with topical retinoids because of his squamous metaplasia. He was referred to me, and I put the him on cyclophosphamide (Cytoxan, Bristol-Myers Squibb). Ten weeks later, the keratin had simply vanished.
If the eye is red hot and rapidly progressive, I treat with cyclophosphamide (Cytoxan, Bristol-Myers Squibb) along with prednisone. Cyclophosphamide is the second-best option to IVIG and rituximab, and it can be given by pulse intravenous dose and converted to daily oral. I use this drug while we’re getting the prior approval on insurance for rituximab and IVIG.
These options give me the flexibility to choose the best treatment for the disease stage and individual patient. OCP is a relatively rare disease, but I see it frequently because of my interest. Again, it is a systemic disease and it demands systemic therapy.

C. Stephen Foster, MD, FACR, FACS, is founder and president of the Massachusetts Eye Research and Surgery Institution in Cambridge; Clinical Professor of Ophthalmology, Harvard Medical School; and Founder and Chairman of the Board of the Ocular Immunology and Uveitis Foundation. |








