Six keys to building the efficient office you want
Smart staffing and optimal use of space will make your practice operate both more smoothly and more profitably.
By Russell G. Fumuso, MD
| About the Author | |
|---|---|

|
Russell G. Fumuso, MD is a founding partner of Ophthalmic Consultants of Long Island. The group operates nine locations, including an outpatient surgical center, on Long Island in New York. His e-mail is rfumuso@ocli.net. |
Good ophthalmic office design creates a space that – along with sufficient staff – supports efficient workflow and enough patient throughput to achieve your practice goals. Five new offices, four office redesigns and three expansions in 30 years have given me clear ideas about how to practice efficiently. Proven office design concepts certainly help, but designing an office is an individualized task. Assessing what you and your partners want from your practice drives what you need from your offices.
Entire books have been written about ophthalmic office design, and covering the topic fully exceeds the scope of this article. Instead, I will focus on six key areas you and any partners should carefully consider in the process of upgrading to an efficient office that is the core of a thriving ophthalmology practice. (This article does not touch on planning for an eye surgery center.)
SIX KEYS
In your quest for efficiency, focus on these points:
1. Assess your current practice. Chances are good that your first thoughts about the need to redesign or expand grow out of the frustration that comes with consistently running behind schedule or not having enough space for all the new testing and ancillary equipment you need for a state-of-the-art ophthalmology office. Patients might grumble about long waiting times, which is universally the number one complaint. Since starting in practice, staying on schedule has been a primary goal for me.
“Am I behind on my schedule?” would be the first question to ask in assessing your practice, but I would bet that you already know that answer. The second might well be whether you are satisfied with your patient volume. If you are frequently behind and want to see more patients, it’s certainly time to consider redesign or expansion. It might be that adding staff could get you back on time and/or enable you to see more patients without adding or reconfiguring space.
Answering questions such as those listed below about your current practice should help you assess whether your current office can meet your practice objectives.
• How often does your practice run behind schedule?
• How far behind schedule does it run?
• How many patients do you see per hour and per day?
• How long does it take from the patient’s appointment time until he or she leaves your office? (Determine this for different types of appointments.)
• How long does it take for a patient to be seen after making an appointment? (If it takes more than a week or two, I think that is a problem.)
• Do you have equipment clogging your hallways?
• Are there services you’d like to provide if you had more space?
These questions assess the practice you have. A more efficient office space, properly staffed, can help you transform the practice you have to the practice you want.
2. Decide what practice you want to have. Once you have developed a good view of the practice you have, the next step is to think about the practice you want to have. From the time I started in medicine 30 years ago, it has been important to me to stay on time. My target has been to see eight to 10 patients per hour, while providing top-quality care.
You also need to consider what services you want to provide. Are there services you want to add to your office? How about equipment? The services you want to provide, including contact lenses and optical, and the number of patients you want to see, greatly influence the amount of space you need to achieve those goals.
3. Renovate, expand or move? Once you’ve measured what your practice is doing and compared it to what you’d like it to do, the key office design question becomes whether your current space can support the necessary changes. If your goal is to see more patients per hour, can you see them in this space? In my experience, the answer is usually no.
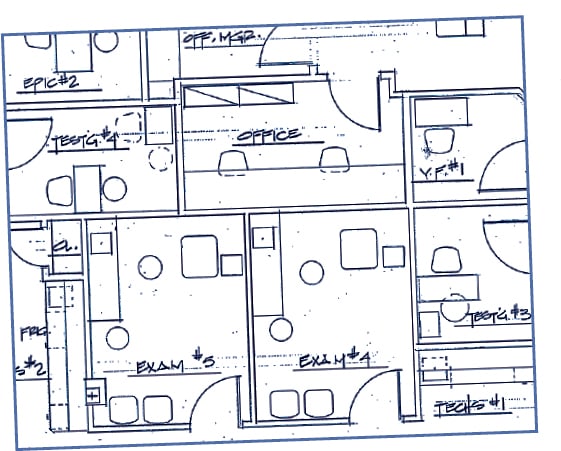
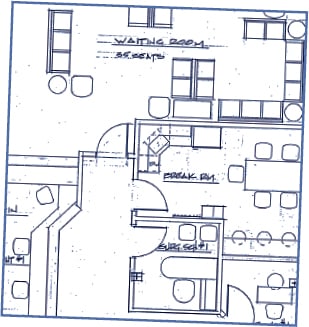
Over the years, we have come up with an estimate of 2,200 to 2,500 square feet for a pod of four exam lanes to support an efficient ophthalmologist. If need be, this number can be reduced somewhat depending on how tightly things have to be packed in. That square footage, designed well, accommodates four 8-by- 12-foot exam rooms (we use mirrors), two testing rooms, an EPIC Refracting System (Marco, Jacksonville, Fla.), waiting and sub-waiting rooms, front desk areas, consultation room, break room and business offices.
Note that the four exam rooms for one ophthalmologist require just over 15% of that 2,500 square feet. In my experience, the utility of the non-exam room space is very important to improving efficiency and seeing more patients. If your current space doesn’t offer similar square footage and exam rooms, you probably need to move unless adjacent suitable office space is available. One of our offices has 10,000 square feet and accommodates 16 lanes along with all the testing and treatment areas, as well as a research department.
This office layout facilitates efficiency with its multiple exam rooms, which help to move patients through the practice and keep doctors on time.

4. Designing space. When it comes to designing office space, I strongly recommend working with an experienced ophthalmic office designer, not just a medical office architect. An ophthalmic office designer will know why a lane needs to be a certain size and will better understand your needs and equipment requirements. A medical architect, on the other hand, may or may not have experience with ophthalmology practices. Your office designer can then work directly with the architect.
The staff’s knowledge of your practice can help you create an efficient office. They certainly know what works and what doesn’t in your existing practice, so they may bring valuable ideas about how to make things run more efficiently.
The exam room is the heart and soul of a practice. You need enough exam rooms to keep patients flowing through (Figure, page 53). You want those rooms filled with patients who have had their testing completed and are ready to see you when you’ve finished with the previous patient. That also requires a sufficient number of testing rooms so you don’t wait in an exam room for a patient to finish a visual field or some other test.
Some of the least efficient practices I’ve seen have huge waiting areas and large, overstaffed front desks, but they didn’t have enough exam rooms. In this day and age, if we want to maintain revenue, we have to see more patients. To do that and still deliver a high quality of care, we need to be more efficient.
Our exam rooms accommodate the patient exam chair, stand, chairs for two accompanying family members, plus a chair for myself and one for my scribe.
So far, I’ve addressed supporting one ophthalmologist working in the office. If more than one doctor will work at the same time, additional pods are needed. Adding a second identically configured pod may work, or you might be able to adjust to slightly fewer testing rooms, depending on doctors’ work rates. I’ve worked on a 5,000-square-foot office with nine exam rooms, five testing rooms and one procedure room. The objective does not change: Move patients through the practice efficiently and have testing completed and the patient ready when an ophthalmologist enters the exam room.
A final design thought: Avoid skimping on space to save small dollars on rent. Losing efficiency, not allowing room for growth or – worst of all – moving into an office that is already too small is a mistake that defeats the purposing of expanding your practice.
5. Staffing. Good design only enables efficiency. You also need enough staff to achieve it.
Ophthalmic Consultants of Long Island utilizes more clinical staff than many practices. I prefer to work with three ophthalmic techs, a testing tech and two scribes. The clinical support staff helps me stay on time and keep patients satisfied with our service. Three technicians provide the staff to keep exam rooms clean and prepared for the next patient, to assist me if needed, and to finish up with the current patient while I move to the next. The testing tech performs needed tests and makes sure the results are in the electronic medical record and on my screen when I enter the exam room.
Since our group converted to electronic health records (EHRs), I’ve utilized scribes to type my notes into he EHR during the exam. Our practice has used NextGen (Horsham, Pa.) practice management software for years and added the company’s ambulatory EHR for ophthalmology several years ago. In my exam rooms, the scribe sits behind and to the side of the patient. We utilize two computer screens, one for the scribe, and one for me. This has proven less distracting to the patient and gives me the ability to display testing to the patient without disrupting the scribe’s note taking. The scribe helps me move faster to the next appointment, finishing up my notes for the medical record after I’ve finished with the patient. This frees me to move to the next patient. The second scribe is ready and waiting for me in the next exam room.
Having scribes handling the data input allows me to spend that time with the patient. After an adjustment period to EHR and scribes, I’ve found that I actually spend more “face time” with a patient then I did when I was hand-writing notes.
Many physicians work with two technicians and don’t use scribes, but if I can see two more patients per hour, that pays for the scribes and extra technician many times over in the course of a year. Younger ophthalmologists raised on computers and who can type really quickly may not need scribe support. Before we had EHR, I did not use scribes and kept to my schedule, but it was tough. Whether your practice uses EHRs or not, how quickly you and your partners can work to deliver quality eye care will determine the staffing needs to work efficiently.
6. Ongoing assessment. Each time we’ve renovated or moved, our practice’s patient volume has increased. My partners and I compile and evaluate practice statistics on each office on a regular basis. Like any good business, you need to assess operations. Setting benchmarks and measuring your actual performance against them helps keep you efficient. Our practice also has targets for exam times, measured from the appointment time until the patient checks out:
• New patient, comprehensive exam: 45 minutes.
• Comprehensive eye exam for an existing patient: 30 to 45 minutes.
• Return follow-up visit: 30 minutes.
From vision to reality
Office design and staffing are two primary tools for bridging the gap between how your office performs and the very efficient practice you envision. Bringing that practice out of your imagination and into reality requires understanding how your office functions, having a clear idea of the practice you want, and using your own and your staff’s experience. Add to those an ophthalmic office designer, staffing the office sufficiently and, finally, monitoring your progress, and you are well on your way to creating the efficient practice you want. OM








