Irregular Corneal Astigmatism and Cataract Surgery
Addressing irregular corneal astigmatism is essential to achieving a good surgical outcome.
BY UDAY DEVGAN, MD, FACS, FRCS (GLASG)
Patients with irregular corneal astigmatism pose additional challenges when performing cataract surgery. Corneal changes may be responsible for a large part of their visual loss and simple cataract surgery may not be enough to restore vision. Depending on the condition and extent of corneal irregularity, the astigmatism may be addressed at one of three time points: before, at the time of or after cataract surgery.
Pre-operative Assessment
All cataract patients should undergo a detailed slit lamp microscopic examination prior to surgery. Significant corneal changes such as stromal scars, pterygia, Salzman nodules, degenerative changes or dystrophies are usually seen well in advance of surgical planning. However, some corneal changes, which induce irregular astigmatism, can be subtle and easy to miss with slit lamp examination alone. Irregular mires on keratometry or curvature values that are outside the normal range alert us to perform further evaluation.
Corneal topography and corneal tomography often provide the best overall assessment of the corneal status and degree of astigmatism, irregularity and symmetry. These platforms can also help in determining the central corneal power to be used in IOL calculations.
Addressing Irregular Corneal Astigmatism Before Cataract Surgery
If the patient has a corneal issue that can be treated before cataract surgery, we should make this the priority. By maximizing the condition of the corneal surface, we’re able to obtain more accurate measurements for IOL calculations and, in theory, a better postop refractive outcome. A pterygium or a Salzman nodule can induce several diopters of irregular astigmatism. Epithelial basement membrane dystrophy (EBMD), also referred to as map-dot-fingerprint dystrophy, can be treated with corneal scraping and smoothing. Even dry eye syndrome can induce a significant degree of corneal irregularity and should be aggressively treated prior to cataract surgery. Patients with a long-term history of contact lens use, particularly rigid lenses, may have corneal changes that can take days or weeks to return to baseline.
For all of these conditions, treatment should be initiated well in advance of cataract surgery and patients should be monitored with serial topography to determine stability. In many of these cases, the cornea can return to regular astigmatism with good symmetry, a condition that is more amenable to treatment at the time of surgery.
Addressing Irregular Corneal Astigmatism After Cataract Surgery
In some patients, corneal astigmatism may be best addressed without surgery. Be aware that patients with mild to moderate corneal irregularities who have been successfully treated with rigid contact lenses, such as some keratoconic patients, may wish to wear their lenses after cataract surgery. When performing cataract surgery, we want to allow them to easily return to their contact lenses without inducing further changes.
Patients with irregularities from prior incisional surgery, such as radial keratotomy, may be best served with a non-toric monofocal IOL and use of rigid contact lenses. In regions where topography-guided excimer laser treatments are available, it may be best to leave certain patients mildly myopic after cataract surgery in preparation for a surface ablative procedure.

Figure 1. If the patient has a treatable cause of preop irregular corneal astigmatism, such as the top patient with a pterygium, address it prior to cataract surgery. If the patient has a highly irregular or unstable cornea, such as this middle patient with severe keratoconus, don’t touch the cornea. If the patient has a symmetric central corneal zone, such as this bottom patient with prior radial keratotomy, then a toric IOL can be a reasonable choice.
Sometimes corneal stromal scars have less effect on the vision than expected. Performing cataract surgery as a first step to achieve better vision is sometimes all that is needed. Remember that if the cornea is highly irregular or unstable, don’t touch it during cataract surgery; any corneal issues can be addressed after surgery. And in some cases, these patients may benefit from a combined corneal transplant and cataract surgery in the same sitting.
If the patient is unlikely to require a corneal transplant in the near future, and if he’s best served by cataract surgery alone, obtaining accurate IOL calculations is important for visual recovery. Care should be taken to use the lowest keratometric values in the central cornea to avoid a hyperopic refractive surprise.
Treating Irregular Corneal Astigmatism at the time of Cataract Surgery
Toric IOLs are powerful tools for addressing corneal astigmatism at the time of cataract surgery, with the ability to treat from 1D to a bit more than 4D of astigmatism. Toric IOLs are machine-made to be perfectly symmetric and regular. Furthermore, because of their inert nature, they’re stable and won’t change over time. These toric IOLs work best in eyes that have very regular, symmetric and stable astigmatism. Note that toric IOLs may also be used in eyes with some degree of irregular corneal astigmatism as long as we adhere to a few guidelines.
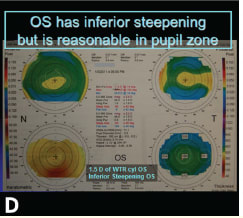
Guideline 1: Look closely at the central corneal topography. Some patients with corneal diseases, such as forme fruste keratoconus or mild cases of pellucid marginal degeneration, can have peripheral corneal irregularities but a reasonable degree of symmetry and regularity of the astigmatism in the central cornea, which encompasses the visual axis. When evaluating the corneal topography, examine the central 3- to 5-mm pupillary zone separately from the peripheral cornea. Patients with symmetric and regular astigmatism in this central zone will likely do well with a toric IOL.
Guideline 2: Select patients who have previously done well with eyeglasses. Spectacles will only correct the spherical (hyperopic or myopic) refractive error and the regular, symmetric refractive astigmatism. Irregular astigmatism cannot be corrected with standard eyeglasses. As such, patients who have recently achieved good vision with conventional eyeglasses must have a fairly regular and symmetric degree of astigmatism in their visual axes.
Guideline 3: Avoid toric IOLs in patients who wish to return to wearing rigid contact lenses. Rigid contact lenses can address corneal irregularities by acting as a new anterior refracting surface of the eye. Thus, patients who wish to return to wearing these rigid contact lenses will be best served by non-toric IOLs. If we implant a toric IOL in a patient who continues wearing a rigid contact lens, it will result in a direct neutralizing of the corneal astigmatism and an immediate unmasking of the toric IOL effect. This type of patient would need eyeglasses and rigid contact lenses to correct the toric IOL. Alternatively, they’ll need to obtain a specialty set of rigid contact lenses that have an anterior toric surface to balance out the now-unmasked toric IOL. The bottom line is this — avoid using toric IOLs in patients who want to continue wearing rigid contact lenses.
Guideline 4: Choose toric IOLs over relaxing incisions in patients with irregular corneas. While we often use limbal or corneal relaxing incisions to address regular, symmetric astigmatism in normal corneas, we should shy away from these procedures when the cornea is irregular. Incisional relaxing techniques can further destabilize a weak cornea and produce even more irregularities.
|
CASE STUDY |
|---|
|
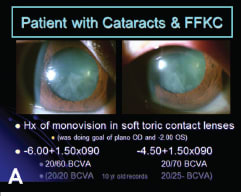
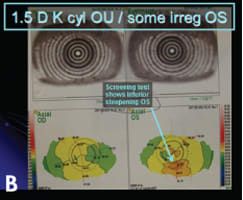
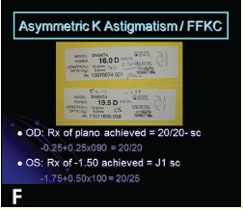
A 62-year-old female is referred to you for cataract surgery due to cortical lens changes that are now in her central visual axis (Figure 2A). She has a history of myopic astigmatism for which she has been wearing soft toric contact lenses for many years in a monovision arrangement. Her medical record over the course of the past 10 years shows a stable refraction with 1.50D of refractive cylinder in each eye. Prior to development of cataracts, with glasses the right eye has been correctable to 20/20, whereas the left eye has achieved 20/25 vision. Screening Placido-disc topography shows regular, symmetric astigmatism of the right cornea whereas the left eye shows inferior steepening (Figure 2B). A more detailed examination of the right cornea confirms the regular and symmetric with-the-rule astigmatism (Figure 2C) with the left eye showing similar central astigmatism but also inferior steepening of the peripheral cornea (Figure 2D). Of particular importance is the pupillary zone of the left eye, which shows central corneal symmetric and regularity. Manual keratometry confirmed the curvature values and showed mild distortion of the mires for the left eye (Figure 2E). A surgical plan was made to use toric IOLs in both eyes to address the corneal astigmatism while keeping a monovision arrangement. The patient achieved excellent vision post-op with the same monovision arrangement, and the best-corrected visual acuities returned to their levels from 10 years prior with the right eye achieving 20/20 and the left eye 20/25 (Figure 2F).
|
The treatment of irregular corneal astigmatism must be individualized to each cataract surgery patient. Fix any issues that can be addressed prior to elective cataract surgery. For highly irregular or unstable corneas, avoid cutting into the corneal tissue to avoid worsening their course. And for patients with milder peripheral corneal irregularities but good central symmetry, consider a toric IOL. By tailoring our treatment regimen to each patient, we can address irregular corneal astigmatism and perform successful cataract surgery to restore vision. ■
|
Uday Devgan, MD, FACS, FRCS(Glasg) is in private practice at Devgan Eye Surgery in Los Angeles. He is chief of ophthalmology at Olive View UCLA Medical Center and Associate Clinical Professor at the Jules Stein Eye Institute at the UCLA School of Medicine. He can be reached at 1-800-337-1969 or devgan@gmail.com for more information.
|