ALT vs. SLT: Is One Better Than the Other?
Each has its place in managing high IOP, but will SLT replace front-line medical therapy?
By Jeffrey S. Eisenberg

Argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT) have been available since 1979 and 2001, respectively, yet ophthalmologists still tend to compare the two procedures. We know that SLT offers several advantages over ALT as far as safety, and that the two procedures appear to be equally effective at managing IOP. But questions remain as to whether SLT is repeatable, and research continues to look at SLT as front-line therapy in place of topical medications.
Key Advantages
In SLT, a 3-nanosecond, Q-switched, frequency-doubled Nd: YAG laser pulse selectively targets melanin granules in pigmented cells of the trabecular meshwork. This offers several advantages over the argon laser. Specifically, SLT:
■ Eliminates coagulative damage to the trabecular meshwork and adjacent structures. It does this by confining the laser energy to the target tissue.1 “There’s more physical damage with ALT,” says Catherine Birt, MD, of the University of Toronto. “It is a hot laser. It heats the tissue and coagulates the tissue. Pathology studies show evidence of more structural damage with ALT than SLT in cadaver eyes.” (Figure 1)
■ Is easier to perform. SLT involves a 400-μm spot size vs. ALT, which involves a 50-μm spot size. “SLT does not require pinpoint focus and pinpoint accuracy of the spot,” Dr. Birt says. “It’s a larger spot size, and you’re painting the whole angle, whereas with the ALT you have to target very precisely the juncture of the pigmented and nonpigmented meshwork. (Figure 2)
■ Is less likely to result in IOP spikes following the procedure. In the past, thermal damage from ALT could lead to IOP spikes of 40 mm Hg or greater within an hour of the procedure. Today, ALT requires less thermal energy, greatly reducing this risk. However, because ALT often requires 50 to 60 spots, the risk is still present. “SLT covers most of the meshwork, but you don’t get the pressure spike. So, even though you’re treating more tissue, you don’t get the pressure rise,” says E. Randy Craven, MD, of Johns Hopkins University’s Wilmer Eye Institute in Baltimore.
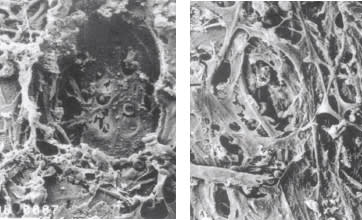
Figure 1. ALT histology (left) shows permanent trabecular meshwork damage while SLT histology shows no destruction of the trabecular meshwork.
“You can actually create glaucoma by doing too much to the meshwork,” adds Cindy M.L. Hutnik, MD, PhD, of the University of Western Ontario in London, Ontario.
Equal Effect …
Since 2001, several studies have shown SLT to be as effective as ALT for lowering IOP. For example, Karim F Damji, MD, of the University of Ottawa Eye Institute, and colleagues, randomized 176 eyes (152 patients with a mean age of 70) that had open-angle glaucoma and uncontrolled IOP of 16 mm Hg or greater on maximal medical therapy (or had previously unsuccessful ALT or SLT) to receive ALT or SLT.2
One year later, IOP decreased an average of 5.6 mm Hg, to 17.97 mm Hg (23.75%), in eyes that underwent SLT, and by a mean 6.04 mm Hg, to 17.88 mm Hg (25.25%), in eyes that underwent ALT. Successful treatment, which researchers defined as a 20% or greater reduction in IOP, was nearly identical: 59.7% of the SLT eyes and 60.3% of the ALT eyes. And, 82% of eyes in the SLT group could remain on the same number of medications at one year vs. 69% of eyes in the ALT group; 18% in the SLT group required one additional drug vs. 29% in the ALT group.
In a follow-up study of the same patients, Dr. Damji and his team found that IOP-lowering effects of SLT and ALT were similar for more than five years in this group of patients.3 IOP in eyes that underwent SLT was lowered by 6.7 mm Hg at three years (28.42%), 7.0 mm Hg at four years (29.65%) and 7.4 mm Hg at five years (32.35%). In those eyes that underwent ALT, IOP was lowered by 6.1 mm Hg at three years (25.5%), 6.3 mm Hg at four years (26.33%) and 6.7 mm Hg at five years (28%).

Figure 2. The larger SLT spots can be placed in the area of the meshwork while the smaller ALT spots must be precisely placed to avoid peripheral anterior synechia.
Mark S. Juzych, MD, of the Kresge Eye Institute and Wayne State University, Detroit, and colleagues found similar results when they compared long-term outcomes of the two procedures.4 In a retrospective study of 195 patients with open-angle glaucoma, 154 eyes had ALT (mean age 70) and 41 eyes underwent SLT (mean age 72). Mean IOP decrease was 18.1% in both groups at one year. At five years, mean IOP decrease was 27.1% in the SLT group and 23.5% in the ALT group. Although the SLT group had fewer patients, the authors still determined that SLT was as effective as ALT in achieving long-term success.
Most of these studies, however, involved older patients. Previous studies, such as the Advanced Glaucoma Intervention Study, have suggested that younger patients were more likely to fail with ALT.5

However, Drs. Birt and Yingwell Liu recently compared ALT and SLT in younger patients. Their prospective, controlled trial randomized one eye in 42 patients ages 29 to 60 to ALT or SLT.6 At two years postoperatively, mean IOP decreased by 11.1% for ALT and 7.7% for SLT. Further, the complete success rate was 45.5% for ALT vs. 40% for SLT. Also, at two years, 86.4% of ALT and 75% of SLT eyes required no further surgical intervention. The data showed no statistically significant difference between the two modalities.
… But Not Superior
James D. Brandt, MD, professor of ophthalmology and director of the glaucoma service at the UC Davis Eye Center, urges caution when interpreting these studies. “None have shown superiority in terms of intraocular pressure lowering or duration of effect,” he says.
“When you’re comparing SLT to ALT it’s critical to make sure that the same type of patient is compared,” Dr. Hutnik adds. Further, ALT may be the more appropriate choice for patients with pseudoexfoliation. “If I have someone with really heavy pigmentation on the meshwork, I will do an ALT,” Dr. Craven says. “SLT doesn’t penetrate the pigment that well.”
But research by Dr. Hutnik awaiting publication may prove otherwise. Dr. Hutnik’s group compared the two procedures in patients with pseudoexfoliation. Her hypothesis: ALT would work much better for penetrating the pigmentation. “Much to my surprise, they worked equally,” she says.
Is it Repeatable?
Another issue surrounds the repeatability of SLT. “There are not very good data about reproducibility. SLT is repeatable in some patients, but so is ALT in some patients,” Dr. Brandt says. “These may be the same patients, and we really don’t know.”
Dr. Brandt’s belief: A successful response to an initial ALT or SLT is truly the best predictor of how well a patient will do on a repeat procedure. He is disturbed, however, when he sees patients with advanced glaucoma who have undergone multiple SLTs even when incisional surgery was warranted, delaying definitive treatment.
Dr. Birt and colleagues have received a grant from the Canadian Institutes of Health Research to conduct a randomized clinical trial of SLT in patients with medically uncontrolled open angle glaucoma who previously had SLT. They anticipate recruiting patients who had one 360° or two 180° treatments in early 2013. The study will run for three years (two for recruitment, one for follow-up). “The null hypothesis is that both lasers are equally effective at lowering pressure in the retreatment mode,” Dr. Birt says.
Dr. Birt, however, believes SLT is the safer choice when retreatment is necessary. “Whereas with ALT, it’s often considered dangerous and not a good idea to treat with ALT and then do a second treatment with the same laser,” she says. Some still argue that ALT remains the gold standard for laser trabeculoplasty.7 Both procedures can cause similar complications, including angle bleeding, transient anterior chamber reaction and pain.
A positive response to either procedure is a predictor that the patient has a reasonable chance of having a good response on a repeat procedure, Dr. Brandt says. His other concern is that some doctors keep attempting SLT even as the patient’s condition worsens and they become more appropriate candidates for incisional surgery. “That’s bad for patients, basically,” he says.
The traditional treatment paradigm has been medication, laser and then surgery. However, the availability of SLT may alter that to laser, medication and then surgery.
ALT as Primary Therapy
Perhaps the real comparison should not be SLT to ALT, but SLT to glaucoma drops. Specifically, can laser treatment be primary therapy instead of medications? In 1990, the Glaucoma Laser Trial established the effectiveness of ALT as primary therapy.8 In this multicenter trial, 271 patients with newly diagnosed, previously, untreated POAG had one eye randomly assigned to ALT and the other assigned to timolol maleate 0.5% (the medication first [MF] eye).
During the two-year follow-up, fewer eyes that received the laser treatment initially required a simultaneous prescription of two or more medications to control IOP than the MF eyes. After two years of follow-up, 44% of LF eyes were controlled by ALT, 70% were controlled by ALT alone or ALT and timolol, and 89% were controlled within the stepped medication regimen. After two years, 30% of MF eyes remained controlled by timolol, and 66% were controlled within the stepped regimen. The Glaucoma Laser Study “certainly suggested that initial laser treatment was safe and effective and very acceptable as a first-line choice,” Dr. Birt says.
| CODING FOR LASER PROCEDURES |
|---|
|
While the efficacy of ALT vs. SLT may be debateable, the billing and coding procedures remain the same. The correct CPT code is 65855 (trabeculoplasty by laser surgery). The correct diagnosis code is in the 365.xx series. “They’re both laser trabeculoplasty. The type of laser doesn’t make any difference. The code is described as laser trabeculoplasty, even though in ophthalmology practices they refer to it as ALT or SLT,” says Suzanne Corcoran, of Corcoran Consulting Group in San Bernardino, Calif. Some additional considerations for coding: • Medicare defines the global period as 10 days. Keep in mind, however, that private payers may have different post-op periods, so check with your plans first. • The multiple procedure rule applies if you perform laser treatment on both eyes simultaneously (although this is rare). Medicare pays 150% of the allowable rather than in full for both eyes, Ms. Corcoran says. • For repeat laser procedures, the same coding rules and 10-day global period apply. |
SLT as Front-Line Treatment
Recent research has focused on using SLT as primary therapy. For example, Madhu Nagar, MD, of Wakefield, UK, and colleagues found no statistically significant difference in success rates for treating patients with SLT vs. latanoprost.9
TABLE: IOP-Lowering of SLT vs. ALT; Three Studies
| Study | Damji et a12,3 | Juzych et al4 | Birt et al6 | |||
| SLT (n=89) |
ALT (n=87) |
SLT (n=41) |
ALT (n=154) |
SLT (n=20) |
ALT (n=22) |
|
| Age | 70 (mean) | 72 (mean) |
70 (mean) |
29−60 (range) | ||
| 1 year | −23.75% | −25.25% | −18.1% | −18.1% | ||
| 2 years | −7.7% | −11.1% | ||||
| 3 years | −28.42% | −25.5% | ||||
| 4 years | −29.65% | −26.33% | ||||
| 5 years | −31.35% | −28% | −27.1% | −23,5% | ||
In another study, researchers assigned 74 eyes to receive SLT and 26 to receive latanoprost as primary therapy.10 One hundred eyes (61 patients) were enrolled, 74 in the primary treatment group and 26 in the control group. The average IOP reductions for the primary treatment group were 8.3 mm Hg, or 31%, in those patients who received SLT vs. 7.7mm Hg, or 30.6%, for the control group.
“My feeling is SLT is like a bottle of eye drops,” Dr. Hutnik says. “It works best when used as primary therapy — an 80% responder rate to achieve 30% IOP reduction from baseline — and second best when used in addition to one drop and third when in addition to two drops.”
More recently, L. Jay Katz, MD, of Wills Eye Institute in Philadelphia, and colleagues randomized 69 patients (127 eyes) with open-angle glaucoma or ocular hypertension to SLT or medical therapy.11 Mean IOP was reduced 6.3 mm Hg, to 18.2 mm Hg, in those who had SLT and 7 mm Hg, to 17.7 mm Hg, in the medication group. At the last follow-up, 11% of eyes had additional SLT and 27% required additional medication. The difference between the SLT and medication groups was not statistically significant. OM
REFERENCES
1. Pham H, Mansberger S, Brandt JD et al. Argon laser trabeculoplasty versus selective laser trabeculoplasty. Surv Ophthalmol. 2008;53:641-646.
2. Damji KF, Bovell AM, Hodge WG, et al. SLT versus ALT: results from a 1-year randomised clinical trial. Br J Ophthalmol. 2006;90:1490-1494.
3. Bovell AM, Damji KF, Hodge WG, et al. Long term effects on the lowering of intraocular pressure: selective laser or argon laser trabeculoplasty? Can J Ophthalmol. 2011;46:408-413.
4. Juzych MS, Chopra V, Banitt MR, et al. Comparison of long-term outcomes of SLT versus ALT in open-angle glaucoma. Ophthalmology. 2004;111:1853-1859.
5. AGIS Investigators. The Advanced Glaucoma Intervention Study: 11. Risk factors for failure of trabeculectomy and argon laser trabeculoplasty. Am J Ophthalmol. 2002;134:481-498.
6. Liu Y, Birt CM. Argon versus selective laser trabeculoplasty in younger patients: 2-year results. J Glaucoma. 2012;21:112-5.
7. Pham H, Mansberger S, Brandt JD et al. Argon laser trabeculoplasty versus selective laser trabeculoplasty. Surv Ophthalmol. 2008;53:641-646.
8. The Glaucoma Laser Trial (GLT). 2. Results of argon laser trabeculoplasty versus topical medicines. The Glaucoma Laser Trial Research Group. Ophthalmology. 1990;97:1403-1413.
9. Nagar M, Ogunyomade A, O’Brart DP, et al. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol. 2005;89:1413-1417.
10. McIlraith I, Strasfeld M, Colev G, Hutnik CM. SLT as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma. 2006;15:124-310.
11. Katz LJ, Steinmann WC, Kabir A, et al . Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma. 2012;21:460-468.








