Hard lessons from Hurricane Sandy one year later
By Bill Kekevian, Senior Associate Editor
COURTESY: DONNA DAVIS
Some practices are still reeling, but what they’ve learned can help you prepare for the next disaster.
Raymond Reich, MD, was not in his Brooklyn office Monday, October 29, 2012, the day Hurricane Sandy swept through his neighborhood, but the fallout changed his life. “It was utter devastation,” he says. Later dubbed “Superstorm” Sandy, its winds and flooding decimated his small, private practice located not far from his Brooklyn home.
“My office was utterly and completely destroyed,” he says with a heavy sigh. “So was my home. So was my son’s home, my other son’s home, and so was my daughter’s home. We were all homeless for about six weeks. The more difficult part was that my livelihood, my medical practice, was also homeless for a similar period of time. That was the economic glue that was able to keep the family running.”
Meanwhile, Donna Davis, administrator at Atlantic Eye Physicians in Long Branch, N.J., had spent the pre-storm hours driving through the nearby town of Sea Bright. Knowing Sea Bright had flood issues, even during normal storms, Ms. Davis wanted to see how the community was preparing. When she saw the entire town shut down, she knew she was facing no ordinary storm. By noon, she would be evacuating her staff.
Both Brooklyn and Long Branch suffered devastating losses. All told, the storm resulted in dozens of deaths and more costs in damages than any US storm besides Hurricane Katrina in 2005. Both storms left medical practices and other community institutions reeling and in search of ways to better prepare for the next disaster.
Practice principals, managers and consultants have developed strategies as a result of these experiences. A year after Hurricane Sandy, a few share lessons learned and lay out warnings for the next disaster.
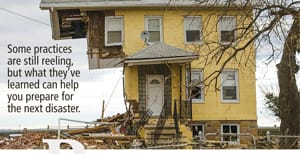
The wreckage in Union Beach, N.J., about 18 miles north of Long Branch, left many without homes or businesses.
DEVELOPING A DISASTER STRATEGY
Steps to writing a plan
“Honestly, most of our disaster plan was developed as we moved through the storm. No one expected it to be so powerful, so each day you plan for the worst and hoped for the best,” Ms. Davis says.
Dave Gans, a senior fellow at the Medical Group Management Association (MGMA) echoes the same sentiment: “Plan for the worst, hope for the best.” That planning part, he says, is the number one lesson any practice manager or physician owner should take from Hurricane Sandy.
A disaster plan should cover four main areas, according to MGMA documents:
- Patient safety. How to best provide for both your patients and the community in need.
- Employee security. How to responsibly keep employees safe. This includes providing appropriate support or counseling following a disaster.
Following the disaster, the plan should focus on:
- Practice capability. When the practice is prepared to return to regular service.
- Financial survivability. How to recoup losses from property damage and practice interruption.
Fortifying your office
The day of the storm, Ms. Davis’s team relocated any piece of heavy, expensive equipment they could from the first to the second floor. This included phaco devices, the biometer and SLT lasers. Staff then notified the IT vendor that the practice intended to power down by noon and requested a confirmation of off-site back-up. Finally, they powered down and unplugged any remaining equipment and took a careful inventory.
Dr. Reich’s practice similarly attempted to protect its valuables. “The night before the flooding, my partner, Ed Rubinchik, MD, hearing that it would actually happen, went to the office to pull out the servers from the basement,” he says. “That saved the day, really. All that patient data was salvaged.”
He also moved several things that he could easily bring home. “Much of the rest was destroyed,” Dr. Reich says. The MGMA advises insurance policies on all heavy equipment, but as Dr. Reich would later learn, insurance isn’t foolproof. (He says his insurance company continues to refuse his claims.)
AS THE DISASTER UNFOLDS
Employee Security
“Make sure to have a phone tree and be certain all staff numbers have been verified and updated,” says Ms. Davis. As practice manager, she saw communicating with staff as her responsibility.
Her practice devised a phone tree. “I called our phone tree, including physicians, and issued a heightened warning that this was not going to be a normal storm. At that point, two of them were already in mandatory evacuated areas. One physician actually needed to be evacuated from his house via boat,” she recalls.
This kind of designated communication is exactly what the MGMA recommends to help keep employees out of harm’s way.
Patient safety
“For a long time, we had a very dysfunctional health system when it comes to emergency planning,” Mr. Gans says. Improvements were “born out of [Hurricane] Katrina. It wasn’t until then that we had a major, citywide disaster that showed all the problems that happen when organizations have not coordinated,” he says.
This brings Mr. Gans to his first point: Practice managers need to get in touch with local hospital systems and other local health care organizations ahead of a disaster. “Oftentimes, a hospital will have a plan,” he says. Large health-care organizations have generally improved their disaster plans since Hurricane Katrina. Getting in touch with these organizations and getting copies of their plans can give you a template for a disaster plan that you can modify for your own needs, he says.
The day of the storm, Ms. Davis says, she “listened intensely to the local authorities as well as monitored the mandatory evacuation areas along the shore. Our oldest and first office is located a block from the shore. On the day we knew the storm was coming, we sent in the office managers and technical supervisors to each location.”
A SUCCESSFUL RECOVERY
Role of reverse planning
“Reverse planning can help you keep the task in perspective,” Mr. Gans says. “Ask yourself what a successful recovery would look like. For example, ask: What would you need to get back to business? Who can help and what resources are available? How can you continue patient care stability?”
Community service: Giving and receiving
Dr. Reich has yet to see a full recovery, but he did receive some help from a friendly competitor. “We had temporary refuge for a short while,” he says. “The chief ophthalmologist of a competing practice located not far from mine but that was unaffected, called me and said ‘I heard what happened. I’m sorry. Our office is not used on Sundays. Do you want to come and use our office? We’d be more than happy to allow you to use our offices all day Sunday and, no, we will not accept any payment.’ We were there for two Sundays and we were able to see people who needed to be seen.”
| Checklist for getting back to business |
|---|
|
The MGMA recommends you make sure these essential systems are running before you return to work following a disaster
“You should not work your recovery alone,” Mr. Gans says. “You’ve got the hospital system, you’ve got other physicians and you have your public health systems, all of which are available to varying degrees.” |

COURTESY: DONNA DAVIS
Like many others, this Sea Bright business braced for the storm and tipped Ms. Davis off to the severity of the oncoming disaster.
The MGMA advises physicians make use of any back-up clinics that will have them and to, in fact, devise a prearrangement. Mr. Gans suggests since many doctors have admitting privileges in nearby hospitals, to take advantage of that relationship, too. You can also make use of your relationship with other practices to help secure staff affected by a disaster.
In the midst of all this, Ms. Davis was able to dedicate time to volunteer for the Red Cross. One of her employees, who asked to remain nameless, was only days away from moving into a new house when the storm hit. Because everything she and her family owned was boxed up and on the first floor, it was all destroyed.
Ms. Davis helped her through it. “Once we finally did get back to work she asked about my family and heard what we’d lost,” Ms. Davis says. “Everyone was giving us gifts. She actually gave us a check for $1,000,” which Ms. Davis says was collected from other staff members who could afford to give.
Practice capability
“We really did not expect to be down that long,” says Ms. Davis. When the practice returned, the surgery center was down an additional 10 days to ensure the back-up generator was filled with gas and running.
Perhaps it goes without saying that a practice requires power before surgery can commence, but one needs to consider other capabilities before a practice can say it’s back up and running after a disaster. These include all communications, confirming a connection to needed financial or insurance institutions, being able to access both patient and staff records (for payroll purposes) and being free from any public health concerns, according to MGMA.
Financial survivability
“We really fared well,” Ms. Davis says. “Our insurance kicked in. We did take a financial hit by having no patients for a little over a week. When we were able to open our doors, we still had a lot of patients who couldn’t get out of their communities.” She says for another whole week patient flow was down to “a tenth of what it used to be.”
In Brooklyn, Atlantic Eye Care’s records were backed up electronically and Dr. Rubinchik was able to retrieve his and Dr. Reich’s servers, but not much else. Almost everything, including much equipment, was ruined, Dr. Reich says.
MGMA suggests purchasing business interruption insurance, a policy Dr. Reich has long held. “When the insurance representative came down, he took one look at the extent of the damages and said ‘We’re not paying for this’ — and they have not,” he says. The insurance company’s offer was “a mere Band-Aid” if he agreed not to seek further payments. He did not have interruption insurance; he had to pay staff and buy new equipment out of his own pocket.
Talk to equipment vendors
Mr. Gans says simply speaking with instrument vendors may be worthwhile after a disaster. For Dr. Reich it was a rare moment of relief. “I got in touch with Don Quinn of Lombart Instruments and told him I needed to set up immediately. They prioritized my order. I had seven new chairs and stands and associated equipment within two or three days,” he says.
“Compared to what my parents had to go through to survive, this was nothing,” he says. “My parents were Holocaust survivors. But compared to normal life, this is a great deal. The orderly organization of life as it preceded for years is not there now. It’s not the way it was. But we’re alive and grateful.” OM
“The orderly organization of life as it preceded for years is not there now.”
— Raymond Reich, MD.








