When a Defect Becomes a Disability
Investigating the impact of glaucoma on visual function in “real world” scenarios.
By David P. Crabb, PhD
The number of people with glaucoma is a growing demographic and the burden of managing patients with the disease is considerable; in the United Kingdom, for example, there are an estimated one million-plus glaucoma clinic visits a year. Assessment of visual impairment in these patients often centers on numbers from measurements used to classify disease state, as performed in an exam room under well-controlled conditions; significantly, however, this neglects the disability resulting from their visual loss. Successful clinical management of glaucoma should equate to correct decisions about intensifying treatment, of initiating intervention, when patients are at risk of developing “visual disability.” Yet little is known about which visual field (VF) defects, at different stages of glaucoma, specifically affect patients' abilities to perform everyday visual tasks.
The ability to link the measurements taken in the clinic to at least an estimate of what patients visually can and cannot do would be enormously helpful to both physician and patient. Moreover, the benchmark for a new treatment success in a clinical trial should be aligned to measurable reduction in visual disability rather than imperceptible changes on a clinical chart. In an attempt to provide these, our research laboratory at City University London (www.staff.city.ac.uk/d.crabb) has been investigating associations between different levels of VF damage in glaucoma and visual disability. Here are some of the findings from our recent studies.
Glaucoma, Visual Disability and QOL
Recently we conducted a systematic review of studies considering visual disability and quality of life (QOL) in glaucoma.1 The importance of these types of studies in glaucoma appears to have been better recognized of late, as the proportion of papers published as a surrogate measure of research activity in the area is increasing. Nevertheless, QOL studies in glaucoma represent only a very small fraction of the total publications in glaucoma research each year. Interestingly, there are fewer QOL articles in glaucoma compared to some other disabling chronic conditions such as rheumatoid arthritis, multiple sclerosis and macular degeneration (Figure 1).
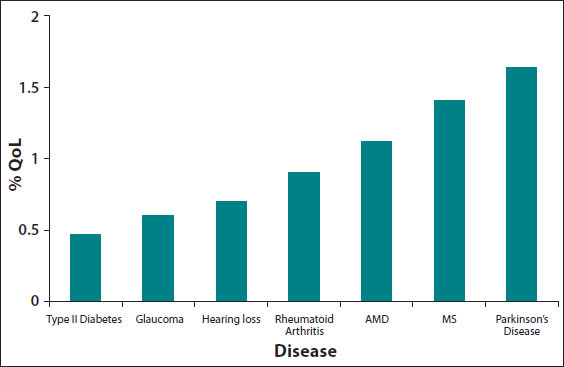
Figure 1. Graph showing the number of QOL studies (on the vertical axis) as a percentage of all studies published for seven chronic diseases over last 10 years.1 This graph suggests that there is less research in this area in glaucoma when compared to other chronic conditions.
The majority of studies examining visual disability and impact on QOL in glaucoma are based on self-report questionnaires. Asking patients how their disease has impacted their ability to do everyday tasks is the best way to ascertain how someone actually feels about his condition. Indeed, much of the best research in the area of visual disability and glaucoma has used this methodology, yielding sound evidence to show that patients with the condition have difficulties with mobility, driving, reading and other everyday tasks. Moreover, there is compelling evidence to show that these problems sometimes manifest in the earlier stages of the disease process, thus contradicting the commonly held belief that glaucomatous patients remain largely asymptomatic until end-stage disease. Excellent reviews of this recent literature are provided by Spaeth (2006) and Ramulu (2009).2,3
But self-report as a measure of level of visual disability is limited by subjectivity, different personal expectations, knowledge of disease and other confounders. Our recent review article, however, illuminated an alternative approach for understanding visual disability in glaucoma by measuring the patient's actual performance in surrogates of tasks they would encounter every day. Tasks previously investigated include mobility performance in terms of ability to navigate around an obstacle course, driving using simulations or direct on-road performance, and examinations of postural sway and balance.
This performance-based approach provides a more objective measure of visual disability and can capture difficulties in performing activities that the individual may not be sufficiently aware of to be able to report them in a questionnaire. 1 The development of objective measures could also potentially offer clinicians a valuable patient-centered method to evaluate disease status and could supplement clinical trial endpoints for justifying the use of new therapies. Research from the Salisbury Eye Evaluation Project4,5 and other groups6 are excellent examples of this approach. We are taking a similar approach in our research laboratory in London.
Our Findings
• Eye-hand coordination in glaucoma. The act of reaching out to grasp an object is a basic, visually-guided task performed many times a day. Accurate and rapid transportation of the hand to the intended target requires precise information about the spatial localization of the object, and this requires both peripheral and central vision. Good vision also drives how we pre-shape the grasp posture and predict the depth of the object relative to the hand to avoid object collision. We recently examined whether patients with glaucoma exhibit differences in visually guided reaching and grasping behavior compared to normally-sighted people.7
Participants in the experiment were required to reach out and precision grasp household objects placed on a table top in front of them. State-of-the-art motion capture units were used to record reflective markers placed on the participant's hand, allowing for accurate measurement of movement in three-dimensional space (Figure 2). Data from these experiments can be used to compose a comprehensive picture of a person's ability to perform this everyday task and the results suggested that patients exhibited deficits in the reaching component, making more tentative movements when reaching for the object. Interestingly, patients with inferior VF defects were particularly susceptible to errors.
Other good data from prospective studies is starting to emerge to indicate that inferior VF deficits are associated with poorer functional status in glaucoma, especially with mobility and movement.8 This is important to note when managing patients with progressive inferior VF defects.
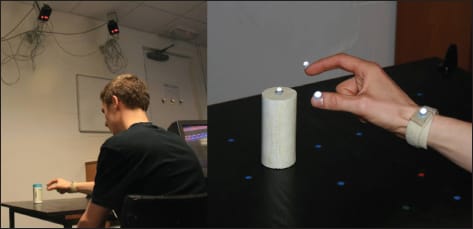
Figure 2. Laboratory set up for the eye-hand coordination experiments.7 ALL IMAGES COURTESY OF THE AUTHOR.
• Searching for objects. One visual task that plays an important role in daily activities that can be estimated objectively is the ability to search for objects in a scene. Indeed, impaired visual search performance will probably place an increased burden on the glaucomatous patient's independent lifestyle, and may be partially linked to the higher number of falls and accidents reported by these patients.
So, in another performance-based experiment, we asked participants to find objects in photographs of everyday scenes on a large computer monitor whilst we tracked their eye movements and recorded the time it took them to successfully find the target (Figure 3). Results indicated that some individuals with glaucomatous VF defects in both eyes find it especially difficult to locate objects when compared to visually healthy individuals of a similar age.9
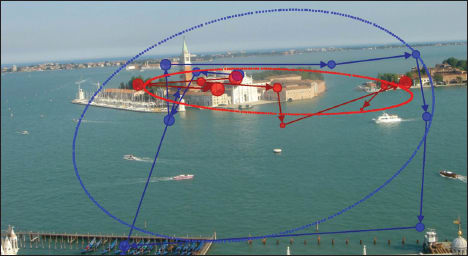
Figure 3. Scan-paths of eye movements (saccades) for a patient (red) and a visually healthy person (blue) searching for a target in a photograph.9 Note that the patient has a more restricted viewing pattern as estimated by the ellipse, which quantifies the area being searched. Some patients with bilateral glaucomatous visual field defects were very impaired when searching for items within pictures.
• Driving and other everyday tasks. Glaucoma undoubtedly has a great impact on an individual when VF loss causes the removal of a driving license. Several studies have shown that certain glaucomatous VF defects are not compatible with safe driving.10 Moreover, in the UK it has been demonstrated that patients regard this particular potential outcome of their disease to be as serious as the long-term risk of blindness.11
The Hazard Perception Test (HPT) is an element of the UK driving license theory test. In the HPT, the “learner driver” is shown a film of a real driving scene, viewed from the perspective of the driver, with the task being to detect potential hazards: These are defined as something that would make the camera car take evasive action, such as braking for an oncoming cyclist or a pedestrian unexpectedly crossing the street. Primarily, it is a useful educational tool allowing learner drivers to encounter “on road” driving scenes from the safety of a computer monitor.
In a recent study, we used the HPT to explore simulated driving performance in patients and simultaneously monitored patient's eye movements using a state-of-the-art eye tracking device.12 On average, patients exhibited different eye movement characteristics to controls, and there were revealing cases where patients failed to see a hazard in relation to their binocular VF defect (Figure 4). The results of this study generated a lot of interest, including an item on the BBC news (Available at: http://news.bbc.co.uk/1/hi/health/7660570.stm. BBC News, UK).
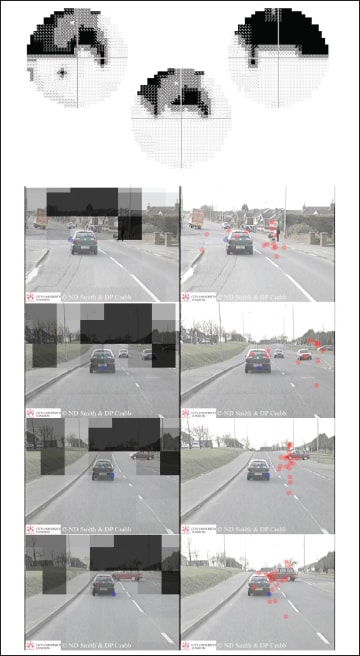
Figure 4. VF grayscales for monocular and binocular integrated visual fields (center)15 for one of the patients who took part in the driving performance study.12 The binocular VF is scaled and superimposed on the point of regard in the HPT film to give a representation of the restricted field of view. The panels show a montage of selected frames from one of the films with points representing the point of regard for all participants. In the top frame, whilst most of visually healthy subjects (red symbols) fixate on the pedestrian, seeing them as a potential hazard, the patient (blue symbol) fails to alter their gaze. In the next frames most of control subjects quickly move their fixation towards the hazard of the car turning on to the main street from the right intersection. (Note that in the UK vehicles are driven on the left side of the road). The patient's view of this hazard is masked by their defect (bottom frame).
• Reading and face recognition. Recently we have been examining more than 100 elderly people, half of whom have a diagnosis of glaucoma, in other lab-based tests. We continue to use the eye movement paradigm in these experiments. These investigations have shown, for example, that patients have difficulty reading passages of text at low contrast. There is little direct association between reading speed and clinically used summary measures of VF defect severity, although patients with quite advanced VF defects in their “better” eye were, on average, slower than age-similar people with healthy vision. A combination of smaller saccade amplitude and increased fixation duration are likely to account for longer reading durations in these patients.
Reading speed is a highly variable measure but analysis of eye movements and examination of specific types of VF defects might reveal more about predicting individual patient's reading impairment. In addition, participants in this experiment have been examined on a face recognition task. There is an association between worsening VF and ability to recognize faces. Moreover, some glaucomatous patients with central 10° VF defects manifest eye movement behavior that is related to better performance in the face recognition task — an association not observed in age-similar people with healthy vision. These findings could be an indicator of how some patients with likely symptomatic glaucomatous damage adapt to VF loss during visual activities. We hope to present these results at the Association for Research in Vision and Ophthalmology meeting in May 2012.
• Binocular visual fields. Because people use both eyes together, a binocular measure is likely the best way to predict the impact of VF impairment on a patient's visual disability. However, in clinical settings, VF resources are dedicated to monocular assessment and binocular testing is rarely carried out. The integrated VF (IVF), developed in our laboratory, offers an alternative assessment of a patient's binocular VF severity.13,14 The IVF is simply estimated from monocular results, taking the best sensitivity values from corresponding VF locations from the two eyes, and requires no extra testing. We have recently shown that monocular VF measures can give the impression that a patient's VF loss is more degraded than it might be under binocular viewing. We propose that the IVF is a rapid assessment of the patient's working VF.15 The IVF is available in the Progressor VF analysis software (Medisoft Ltd., Leeds, UK).
New Measures Needed
An important goal for the research showcased in this article is to develop potentially better outcome measures for clinical trials. In ophthalmology, most of these have concentrated on visual status as a measure of treatment success, whether it be an improvement in resolution vision (visual acuity) or a reduction in the progression of VF defects. However, compared with clinicians, patients have different endpoints as a measure of their treatment success — specifically, how their vision interacts with other conditions and whether they will be able to lead a personally satisfying life. Our lab in London, using expertise in visual science, ophthalmology, psychology and statistics, is aiming to set a foundation for these outcome measures and to stimulate others to derive tests that can be used for this purpose.
In the meantime, tools like the binocular IVF should help clinicians initiate a conversation with their patients about how impairment from glaucoma directly affects their vision. It is important, based on current research findings, that those conversations include driving a motor vehicle, the risk of falls, and problems with mobility and other everyday visual tasks, such as reading and face recognition, especially as the disease process gets more advanced. OM
References
1. Glen FC, Crabb DP, Garway-Heath DF. The direction of research into visual disability and quality of life in glaucoma. BMC Ophthalmol. 2011;11:19.
2. Spaeth G, Walt J, Keener J. Evaluation of quality of life for patients with glaucoma. Am. J. Ophthalmol. 2006 Jan;141(1 Suppl):S3–14.
3. Ramulu P. Glaucoma and disability: which tasks are affected, and at what stage of disease? Curr Opin Ophthalmol. 2009 Mar;20(2):92–8.
4. West SK, Rubin GS, Munoz B, Abraham D, Fried LP. Assessing functional status: correlation between performance on tasks conducted in a clinic setting and performance on the same task conducted at home. The Salisbury Eye Evaluation Project Team. J. Gerontol. A Biol. Sci. Med. Sci. 1997 Jul;52(4):M209–17.
5. Freeman EE, Broman AT, Turano KA, West SK. Motion-detection threshold and measures of balance in older adults: the SEE Project. Invest. Ophthalmol. Vis. Sci. 2008 Dec;49(12):5257–63.
6. Warrian KJ, Altangerel U, Spaeth GL. Performance-based measures of visual function. Surv Ophthalmol. 2010 Mar 4;55(2):146–161.
7. Kotecha A, O'Leary N, Melmoth D, Grant S, Crabb DP. The functional consequences of glaucoma for eye-hand coordination. Invest. Ophthalmol. Vis. Sci. 2009 Jan;50(1):203–13.
8. Black AA, Wood JM, Lovie-Kitchin JE. Inferior visual field reductions are associated with poorer functional status among older adults with glaucoma. Ophthalmic Physiol Opt. 2011 May;31(3):283–91.
9. Smith ND, Crabb DP, Garway-Heath DF. An exploratory study of visual search performance in glaucoma. Ophthalmic Physiol Opt. 2011 May;31(3):225–32. 10. Haymes SA, LeBlanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Glaucoma and on-road driving performance. Invest. Ophthalmol. Vis. Sci. 2008 Jul;49(7):3035–41.
11. Bhargava JS, Patel B, Foss AJE, Avery AJ, King AJ. Views of glaucoma patients on aspects of their treatment: an assessment of patient preference by conjoint analysis. Invest. Ophthalmol. Vis. Sci. 2006 Jul;47(7):2885–2888.
12. Crabb DP, Smith ND, Rauscher FG, Chisholm CM, Barbur JL, Edgar DF, et al. Exploring eye movements in patients with glaucoma when viewing a driving scene. PLoS ONE. 2010;5(3):e9710.
13. Crabb DP, Viswanathan AC. Integrated visual fields: a new approach to measuring the binocular field of view and visual disability. Graefes Arch. Clin. Exp. Ophthalmol. 2005 Mar;243(3):210–216.
14. Owen VMF, Crabb DP, White ET, Viswanathan AC, Garway-Heath DF, Hitchings RA. Glaucoma and fitness to drive: using binocular visual fields to predict a milestone to blindness. Invest. Ophthalmol. Vis. Sci. 2008 Jun;49(6): 2449 –2455.
15. Asaoka R, Crabb DP, Yamashita T, Russell RA, Wang YX, Garway-Heath DF. Patients have two eyes!: binocular versus better eye visual field indices. Invest. Ophthalmol. Vis. Sci. 2011 Aug;52(9):7007–11.

|
David Crabb, PhD, is Professor of Statistics and Vision Research at City University London. He is a fellow of the Royal Statistical Society, honorary consultant in Visual Science at Moorfields Eye Hospital and the leader of the Applied Vision Research Group at City University. Contact him via email at d.crabb@city.ac.uk. |








