Surgical Interventions
A study shows that minimally invasive surgery benefits certain glaucoma patients.
While trabeculectomy remains the gold standard for IOP-lowering surgery, the drive to develop an equally efficacious and more reproducible procedure with a more favorable long-term success rate and adverse event profile continues. This has led to the availability of several viable and increasingly used alternatives. A number of procedures and devices designed to open or bypass the eye's natural drainage system can now be considered for improving aqueous outflow in patients with progressive optic nerve damage or whose IOP is not adequately responding to topical and laser therapy.
“Having options for primary glaucoma surgery is certainly advantageous, but we have more to learn about where each should fit into the disease and treatment continuum and which procedures are best-suited for which patients,” says Malik Y. Kahook, MD, associate professor of Ophthalmology at the University of Colorado. “My patient population is not typical. I see mostly advanced glaucoma in a tertiary care center, and these patients require low postoperative pressures.
Therefore, I use trabeculectomy or glaucoma drainage device implants more often than other surgical procedures. I believe there is a role for minimally invasive glaucoma surgeries, particularly the ab-interno devices and procedures, in patients with moderate glaucoma, especially when combined with cataract extraction. I have adopted some of these new procedures in my surgical practice.”
Rather than utilize every available new device and procedure, Dr. Kahook prefers to decide which options to adopt based on the available evidence of safety and efficacy, the usefulness in particular patient populations, and the outcomes reported in peer-reviewed literature. “The Express Glaucoma Filtration Device (Alcon Laboratories) is one such device that I have found to be valuable for particular patients in my practice, says Dr. Kahook.
To evaluate the performance of the Express device in his own practice, Dr. Kahook conducted a retrospective, consecutive case-control series.1 He analyzed several postoperative outcome metrics from 35 consecutive Express procedures and 35 consecutive trabeculectomies with at least 2 years of follow-up. Mean follow-up was 28 months ±3.23 months. The numbers of phakic, aphakic and pseudophakic patients in the study were similar. In all of the Express cases, a fornix-based approach and a 3x3 mm scleral flap were used, and the P-50 model of the device was inserted with a 27-gauge needle. Complete success was defined as IOP greater than or equal to 5 mmHg and less than or equal to 18 mmHg and at least a 30% decrease in IOP without the use of medications. Qualified success was defined the same as complete success but with use of IOP-lowering medications. The results were as follows:
► Complete and qualified success rates were similar between the two groups. Among Express cases, 77.14% met the definition of complete success vs. 74.29% in the trabeculectomy group (p=1.00). An additional 5.71% and 8.57% met the definition of qualified success for Express and trabeculectomy, respectively (p=0.99).
► The extent of IOP-lowering was also similar between the groups. Final IOP represented a 45.15% decrease from baseline in the Express group and a 48.45% decrease from baseline in the trabeculectomy group (p=0.209). Baseline pressures had been slightly higher in the Express group. Postoperatively, IOPs were similar in the two groups up to 1 year. By the end of follow-up, IOP in the Express group was slightly higher than in the trabeculectomy group.
► The Moorfields Bleb Grading system (MBGS) was used to compare bleb morphology between the two procedures. Vascularity was lower in the Express group for much of the follow-up period. However, by one year to 18 months after surgery, it was equal between the two groups. Bleb height followed a similar course. Until approximately 18 months postoperatively, the Express blebs were lower and more diffuse than the trabeculectomy blebs, but by the end of follow-up the differences dissipated.
► Patients in the Express group returned to their baseline best-corrected visual acuity one week after the procedure, while patients in the trabeculectomy group did not return to their baseline BCVA until 1 month post-op.
► The number of complications was lower in the Express group, but not significantly different from the trabeculectomy group. For example, hypotony occurred in two Express patients and five trabeculectomy patients (p=0.428). Hyphema occurred in one Express patient and four trabeculectomy patients (p=0.356).
► The mean number of glaucoma medications used after surgery did not differ significantly between the two groups. The mean number of medications used preoperatively was 2.29 (SD=0.75) in the Express group and 2.25 (SD=0.77) in the trabeculectomy group (p=0.826). At last follow-up, the mean number of medications used was 0.15 (SD=0.35) in the Express group and 0.20 (SD=0.41) in the trabeculectomy group (p=0.585).
► While long-term outcomes, as described above, were similar in both groups of patients, those who underwent the Express procedure required fewer office visits for the first three months postoperatively, 6.05 (SD=0.54) compared with 8.23 (SD=0.92) in the trabeculectomy group (p<0.000).
► The retrospective case series also highlighted the fact that Dr. Kahook was more likely to perform laser suture lysis sooner in Express patients, “perhaps because I was less concerned about the risk of very low pressures due to the flow regulation provided by the Express,” he says.
Dr. Kahook's Surgical Treatment Algorithm
For Dr. Kahook, the results of the study confirmed that the Express device is a worthwhile addition to the surgical options he offers to his patients. Based on the study findings and his experience to date, the procedure he chooses for each patient requiring surgery for the first time hinges on the target IOP (Figure 1). If pressure in the mid to high teens is the goal, and the patient has a cataract, it is often possible to achieve and sustain the target IOP with phacoemulsification alone, he says. If cataract surgery alone is not sufficient, Dr. Kahook's next choice is to combine it with Trabectome, endocyclophotocoagulation (ECP) or the Express device. If the patient is pseudophakic, he is less likely to choose standalone ECP or Trabectome.

Figure 1. The decision to use minimally invasive surgical procedures for glaucoma depends on the stage of disease and target pressure. Newer procedures and devices are typically utilized for mild to moderate disease and are often combined with cataract surgery.
If the target IOP is lower than the mid to high teens, 12 mmHg for example, Dr. Kahook considers either trabeculectomy or the Express device. “Express is a higher-cost procedure, which is an important consideration,” he says. However, he prefers it over trabeculectomy for particular patients, including:
► highly myopic patients who are prone to hypotony (The flow regulation the device provides helps to prevent this complication.)
► combined Express and cataract surgery (Because no iridectomy is required with the Express device, eyes are quieter postoperatively, which seems to correlate with faster visual recovery.)
► monocular patients (It is crucial for them to regain visual acuity as quickly as possible.)
► patients on anticoagulation medications (Avoiding iridectomy should reduce the risk of hyphema.)
Developments on the Horizon
“In the not-too-distant future, we may have even more glaucoma surgical options to compare and contrast,” Dr. Kahook says. “IOP-lowering systems such as CyPass (Transcend Medical) and iStent (Glaukos), already in use outside the United States, will likely come before the FDA for approval. While long-term efficacy has yet to be determined, our European colleagues report these devices are not difficult to implant at the time of cataract surgery, can decrease IOP more than cataract surgery alone, and appear to have a very low risk for complications. Newer devices such as these could provide opportunities for earlier surgical intervention, which we may ultimately find to be advantageous for our patients.”
Dr. Kahook also points out another development on the horizon: the concept of combining minimally invasive glaucoma surgical devices with drug delivery capability. “Ideally, this would allow us to lower IOP as effectively as with trabeculectomy, but without the associated risk of complications,” he says. “The future of glaucoma surgery is bright and our options are expanding.”
Reference
1. Good TJ, Kahook MY. Assessment of bleb morphologic features and postoperative outcomes after Ex-PRESS drainage device implantation versus trabeculectomy. Am J Ophthalmol. 2011;151:507-513.
Dr. Kahook is involved in the development of glaucoma surgical devices with intellectual property licensed to ShapeOphthalmics LLC and ShapeTech LLC.
| Surgical Pearls for the Express Glaucoma Filtration Device |
|---|
| Dr. Kahook offers the following advice for implanting the Express Glaucoma Filtration Device. 1. After creating the scleral flap, use a 27-gauge needle to make the sclerostomy tunnel for insertion of the Express. I prefer this size needle because it provides a tighter fit around the device, preventing leakage. (Other surgeons prefer different sizes.) 2. Remove the 27-gauge needle from the eye slightly tangentially, leaving a partial thickness side slit in the sclera, so the device can more easily fit into the site. 3. Make the entry site into the anterior chamber slightly posterior to the blue line, about 0.5 mm, instead of close to the cornea as was originally recommended. The added scleral support gives the device more stability. 4. After inserting the device, ensure it is flush with the sclera; otherwise, conjunctival irritation or erosion will be an issue. 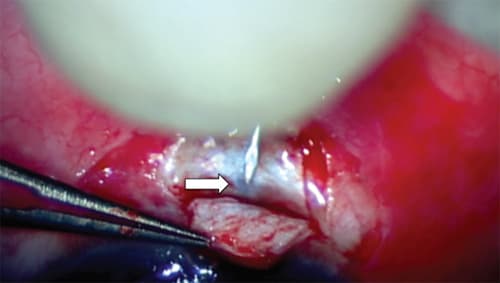
A 27-gauge needle is used to create a sclerostomy tunnel approximately 0.5 mm behind the blue line (arrow) for insertion of the Express Glaucoma Filtration Device. This allows for greater scleral support around the device and less mobility. |








