Surgery with Preexisting Corneal Conditions
Four problems predispose patients to complications or diminish outcomes from cataract surgery.

By John A. Hovanesian, MD, FACS
Preexisting corneal conditions can predispose patients to complications or subpar outcomes from cataract surgery. Those conditions generally fall into two categories: 1) those that represent a risk of significant loss of visual acuity after surgery, such as Fuchs' dystrophy, and 2) conditions that lessen patient satisfaction, such as dry eye, epithelial basement membrane dystrophy, and Salzmann's nodular degeneration.
Patients need to know about their problem before surgery, not after. If you're targeting a precision outcome with cataract, don't hesitate to make a patient wait to get an accurate reading. The old adage, “Measure twice, cut once,” certainly applies. If patients are impatient, put the wait in perspective. They usually don't mind repeating measurements to get a more predictable surgical outcome.
Fuchs' Dystrophy
The danger of Fuchs' dystrophy for cataract surgery patients is that this abnormality of the cornea's endothelial cells, recognizable on specular reflection as excrescences on the interior surface of Descemet's membrane, causes loss of vision through forward light scatter. This leads to reduced contrast acuity and even Snellen visual acuity when bumps are dense and central. More advanced Fuchs' dystrophy causes temporary or permanent endothelial decompensation following cataract surgery.
A careful slit lamp exam prior to cataract surgery should always include seeking abnormalities on specular reflection, including Fuchs' dystrophy. When in doubt, pachymetry and specular endothelial cell counts can help you stratify risk. Less than 1,000 cells per square millimeter and central pachymetry greater than 600 microns are warning signs of increased risk of decompensation.
In the past, the presence of Fuchs' dystrophy prompted us to delay cataract surgery in order to defer risk. Now we don't delay surgery, but rather intervene sooner to prevent endothelial damage from an overly sclerotic nuclear cataract. We find that patients with Fuchs' are less likely to decompensate if we remove the cataract earlier, when phacoemulsification requires less energy. Still, most corneas with at least moderate Fuchs' Dystrophy decompensate to at least some degree after surgery. It's wise to wait at least 2 to 3 months before determining that endothelial replacement surgery is necessary.
Dry Eye
The goal of taking measurements before cataract surgery is to allow the best, most accurate measurements possible, which will result in a very precise surgery. The surface of the cornea is integral to those preoperative measurements, which is why before we take those measurements, we need to optimize the condition of the ocular surface. The goal is to normalize tear volume, consistency and breakup time.
We have a number of tools to help us address dry eye before cataract surgery. Artificial tears can help mild cases, and punctal plugs improve tear volume and normalize the ocular surface fairly quickly. Patients with meibomian gland dysfunction respond to azithromycin (Azasite, Ista Pharmaceuticals). If a patient has severe dry eye, a more aggressive approach is necessary, incorporating multiple modalities simultaneously. It's also sensible to encourage patients to do their own trial-and-error work; if something works in one eye, then use it on both. Therapies such as flax oil and cyclosporine (Restasis, Allergan) take weeks to work, so they're better for long-term treatment of dry eye after surgery.
Treating dry eye before cataract surgery delays surgery for a week or two, but one must remember that patients adhere to dry eye treatment best shortly after they begin a new treatment. After a few weeks, as treatment begins to interfere with their lifestyles, compliance falls off. Treat the dry eye, obtain better measurements after a week or two, and proceed with surgery.
Epithelial Basement Membrane Dystrophy
Like dry eye, epithelial basement membrane dystrophy (EBMD) can affect the validity of keratometry measurements, so we need to treat it before surgery as well as after, or it will likely reduce predictability and patient satisfaction. Like dry eye, EBMD can be revealed by a careful exam, where one finds map areas, fingerprint lines, and dots of epithelial microcysts—all classic harbingers of this common epithelial dystrophy.
To treat EBMD, consider epithelial debridement, use of corneal burr, and phototherapeutic keratectomy (PTK), especially if the patient has erosive symptoms. If there is significant abnormality in the central cornea, I prefer debridement at least 1 month before preoperative biometry is performed. I remove the epithelium, then use a corneal burr to move over the entire de-epithelialized surface for about 10 seconds to remove residual basement membrane, and finally do therapeutic keratectomy, applying 20 to 30 spots of a broad, circular beam while moving the patient's head in a circular fashion to “paint” the laser treatment over the entire exposed surface of Bowman's membrane.
Salzmann's Nodular Degeneration
Salzmann's nodular degeneration (SND) crosses the barrier between preexisting corneal conditions that risk the loss of visual acuity after surgery and those that simply threaten patient satisfaction. Mild peripheral cases may have minimal impact on vision, whereas more advanced or centrally involved cases may have significant large, central distortion of the corneal topography, which can greatly reduce the accuracy of preoperative measurements. A 1-diopter error in preoperative keratometry results in a 1-diopter error in the refractive outcome, so we need to address this problem any time it is likely to affect keratometry.
We treat SND by removing the nodules, scraping them from the surface with the side of a #15 blade scalpel, and allowing the surface to heal. Over the next few weeks, remodeling of the epithelium occurs. In my experience, if we remove a large lump, we see that the epithelium and to some extent the stroma, have remolded around the bump, and it takes time for the eye to find its final curvature and for the surface of the epithelium to normalize.
Treating SND delays surgery by at least a month, but most patients are more than willing to delay their procedure in the interest of a better outcome.
During Surgery
All pre-existing corneal conditions require a bit of careful handling during cataract surgery. In all cases, try to minimize epithelial trauma to reduce any potential healing difficulty.
In patients with Fuchs' dystrophy, use a dispersive OVD with chondroitin sulfate, keep the bottle height low, make sure the incisions are tight (no leaks), and avoid moving instruments in and out of the eye to prevent chamber collapse.
Pre-existing conditions can influence your choice of IOL as well. Do not use a multifocal lens for patients with imperfect corneas from Fuchs' dystrophy or dry eye because of the light scatter associated with those problems. Instead consider a neutrally aspheric IOL or a monofocal approach. You can use an accommodating lens such as Crystalens (Bausch + Lomb) if the patient has adequate visual potential (≥ 20/25). These lenses have good results in patients with compromised contrast.
Postoperative Care
After surgery, patients need a steroid and an NSAID to reduce pain and inflammation. I have used generic prednisolone acetate from a variety of manufacturers, but the particles can become captured in the bottle, and drop size varies. Brand name prednisolone acetate (Pred Forte, Allergan) is more consistent. Difluprednate (Durezol, Alcon) is a stronger steroid delivered in an emulsion rather than a suspension, which produces greater consistency in drug delivery.
All of our NSAID choices are good. The strongest compound is bromfenac (Bromday, Ista Pharmaceuticals), whose potency on cyclooxygenase receptors is several times that of the competing compounds. It is effective and dosed only once a day for better convenience and possibly better compliance.
Be sure to educate your patients about avoiding generic medications, especially NSAIDs, given their past association with corneal melting and predisposition to lead to continued punctate corneal staining and reduced visual quality. With generics, we don't know what patients are getting, and the generic ingredients may not have been studied thoroughly. The complications we've seen arise from generic drugs are virtually unheard of with branded medications.
Patients' Patience
Many patients hear that their friends' cataract surgeries were fast and easy. A patient with a complicated cornea wonders, “Why do I have to wait a month for surgery? Should I go to another doctor?”
Encourage patience in your patients. Not everyone has the same trouble-free road to cataract surgery; some patients require treatment beforehand to get the best results. Treatment will eliminate symptoms that the patient may have been living with for years anyway. This group of patients with pre-existing conditions needs more education and hand-holding before and after surgery. In my practice, we have an effective group of primary care optometrists who share care of cataract patients and can manage them postoperatively, except in problem cases that require the surgeon's involvement.
As always, set expectations for a longer recovery in patients with comorbidities such as corneal abnormalities. If patients recover ahead of schedule, it's a bonus. Encourage them to work with you, diligently holding up their responsibilities with medications and recommendations after surgery to enjoy the full results of the procedure.
John A. Hovanesian, MD, FACS, is a clinical instructor at the Jules Stein Eye Institute, UCLA, and is in private practice at Harvard Eye Associates in Laguna Hills, Calif.
| Patients with Endothelial Disease Deserve Special Attention A dozen tips to help ensure the best cataract surgery outcomes when patients have endothelial disease |
|---|
1. Assess every cornea 2. Consider endothelial cell counts in all premium IOL patients 3. Beware of automated cell counts 4. Heed the predictors of decompensation 5. Counsel preoperatively 6. Be careful with presbyopia-correcting implants 7. Take your time in surgery 8. Tailor your approach to the situation 9. Minimize fluid turnover 10. Consider chilled BSS Plus (Alcon) 11. Work “in the bag” 12. Take steps postoperatively 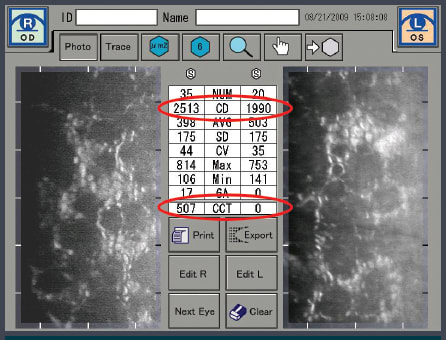
Beware of automated cell counts. 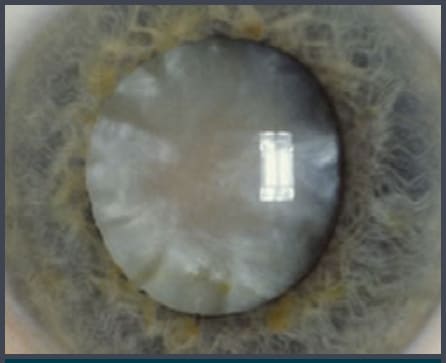
With endothelial disease, cataract surgery is generally done safer, sooner. |








