LASIK Complications: Fact vs. Fiction
Advances have vanquished many of the old bogeymen, but some potential problems remain.
BY RENÉ LUTHE, SENIOR ASSOCIATE EDITOR
The announcement last fall that the FDA was embarking on a study of quality of life for the popular LASIK procedure has brought renewed attention to the negative publicity directed at it by a group some call a vocal minority. This type of publicity seems to come in waves, which might lead the public to conclude that refractive surgery is a procedure beset with ongoing complications. Yet leading surgeons contend that the reality is almost the polar opposite: serious LASIK complications have become rare and are growing more so every year. Here, refractive surgeons separate fact from fiction.
Better Tools
Many of the worst horror stories on the “LASIKRuinedMyLife.com”-type Web sites are attributable to mistakes that occurred in the earlier days of refractive surgery, Mark E. Johnston, MD, FRCSC, medical director and chief surgeon at Nebraska Laser Eye Associates in Omaha, points out. “They are talking about something that happened 10 years ago, maybe even 15 years ago, and they're still mad. I think the big story is that serious complications are extremely rare.”
A big difference between then and now, surgeons note, is the superior technologies available. The femtosecond laser is chief among them. Mark Terry, MD, of Devers Eye Institute in Portland, Ore., notes that it has largely eliminated intraoperative complications such as buttonholing, corneal scarring and damaged flaps.
“The use of femtosecond laser has led to corneas that are more structurally stable than in the past, when the bladed keratomes disrupted the anterior corneal lamellae with a deeper cut,” explains Andrew E. Holzman, MD, medical director for TLC Laser Eye Centers in McLean, Va.
Striae of the flap, he says, is largely eliminated with careful attention to detail in placing the flap into its bed — which femtosecond facilitates — as well as adequate lubrication in the immediate postoperative period.

COURTESY OF WILLIAM TRATTLER, MD.
Incomplete LASIK flap, with scarring within the visual axis.
Additionally, he points out, elevation-based mapping systems help surgeons identify inappropriate candidates, such as those with steepness of the posterior cornea that's believed to be a sign that ectasia could develop after LASIK surgery, or those with early keratoconus.
Finally, newer generation phakic IOLs give surgeons an option for highly myopic patients, saving them from complications that would almost surely come with laser surgery.
Better Therapeutics
“Hyperosmotics pre-op is the norm in my LASIK practice; we believe this helps to reduce epithelial-induced inflammatory conditions postoperatively” Dr. Holzman says. He also uses both steroids and non-steroidal medications. He begins the patient on Xibrom BID one day preop, continues for the first three days postop, and then adds Pred Forte Q2h for the first day postop followed by QID for the rest of the week. “These medications work synergistically by attacking both arms of the prostaglandin cascade, thereby reducing inflammation better than either one alone.”
For patients at risk for dry eye, many surgeons will prescribe cyclosporine two to three weeks preoperatively.
Better Techniques
But better refractive surgery results aren't just the product of improved lasers and medications. Inevitably, there is the human element. “I think what we have seen since I started doing refractive surgery 15 years ago is that every year, you just do a little better — every year over year over year, we learn little things,” Dr. Johnston explains.
He draws an analogy with golf. “You can be the world's best golfer, but every year — since young people are coming along, since expectations are high — you might need to take a quarter stroke off your average. You need to be that little bit better. And every year, we do a little bit better. Because the technology improves a little bit, and our techniques improve a little bit and our knowledge improves a little bit.”
What Remains
“What I tell my patients is that there are side effects” to refractive surgery, explains Ronald Krueger, MD, medical director of the Department of Refractive Surgery at Cleveland Clinic's Cole Eye Institute.
Dr. Johnston takes a similar approach. “When you use that term, ‘complication,’ I think you're talking about something significant and long term, and in our experience, many of the problems I've reported as adverse events were not necessarily complications,” he says.
The lesser problems, or side effects, that remain for patients and surgeons to deal with are the following:
■ Dry eye. “We expect that some patients will have transient dry eye symptoms after surgery,” Steven C. Schallhorn, MD, chief medical director of Optical Express and in private practice in San Diego, explains. “It's part of the healing process.” This transient dry eye is not something that is characterized as a significant complication. However, significant dry eye symptoms that persist longer than one would expect of the normal healing process could be.
Therapies for dry eye have been covered extensively elsewhere, but include punctal plugs, artificial tears, cyclosporine and agents such as AzaSite and doxcycyline for blepharitis and/or meibomiam gland problems. Dr. Krueger recommends the use of a gas permeable contact lens in some cases, because it protects the surface of the cornea and allows that surface to heal without the dryness factor by providing a layer of moisture beneath the lens.
“The plugs go into the drainage tubes; we put those into the upper and lower punctum, or canaliculis. Because they are in the canaliculis, they are not on the outside of the eye, to rub on the eye, which is always a concern right after surgery.”
However, Dr. Johnston points out that what many think of as dry eye syndrome is really a mild neurotrophic keratitis, caused by cutting the nerve endings during refractive procedures. This condition gets better, he says. “The nerves grow back.” The extended intracanalicular plugs in both eyes following surgery help these patients, too.
But careful preoperative screening is still key. “If we look carefully, we'll sometimes see the patients who struggle a bit after surgery are the ones we were not as vigilant in screening out the potential for these problems beforehand,” says Dr. Krueger.
“We look very carefully at the cornea,” Dr. Schallhorn says. Patients who have signs and/or symptoms of dry eye are treated until resolution; if it doesn't resolve, they are not considered appropriate candidates for LASIK.
■ DLK. The most common complication after dry eye, Dr. Schallhorn says, is mild deep lamellar keratitis (DLK). At Optical Express, the incidence is one in 500. He treats it with “intense topical steroids” and it typically resolves quickly.
The more severe inflammation of stage 3 or 4 DLK can be sight-threatening and lead to reduced BCVA, Dr. Holzman notes. Treatment might require a flap lift or oral steroids. However, severe DLK occurs much more rarely Dr. Schallhorn says. He estimates it at one in 4,000 patients. “As with most other complications today, prevention is the key to avoiding them,” Dr. Holzman says. “Attentive detail to ensuring epithelial integrity decreases the risk of epithelial disturbance and therefore also reduces DLK risk.”
“While the technology has improved the architecture of the surgery, making intraoperative complications rare, post-operative complications such as infections and DLK can still occur, of course,” says Dr. Terry. The challenge, he says, is to recognize whether the DLK is infectious or noninfectious. “That's difficult because noninfectious DLK can mimic the infectious process of an actual interface infection,” he explains. “If there is even the consideration that you have an infectious process going on, you are obligated to determine if it is infectious.”
He advises lifting the flap and doing a culture when severe inflammation is observed. “The infections happen most likely during the surgery but they can also happen in the immediate postoperative period,” Dr. Terry warns.
“Infection thankfully is very rare in our practice,” says Dr. Holzman. “We use preoperative fluoroquinolones pro-phylactically, and are careful in pre-treating lid and surface conditions which predispose the patient to keratitis.”
■ Night vision problems. Night glare and halos after LASIK are now a rare problem. The most common cause, says Dr. Schallhorn, is uncorrected refractive error. Such patients are managed with glasses, contact lenses or retreatment. “What a lot of people see, when they are out of focus, is halo around lights,” Dr. Johnston points out. Neither surgeon views this cause of night vision problems as serious.
However, glare or halos despite correction for sphere and cylinder can occur. A custom treatment can be used to address these higher-order aberrations, according to Dr. Schallhorn.
Dr. Krueger, on the other hand, says that repeat customized ablations are not always the answer, because the surgeon has already obtained the desired refractive correction; to do more would detract from the emmetropic result. Instead, he recommends glaucoma drug Alphagan, for its slight pupil-constricting properties.
“That could help if a patient has to go out in the evening,” he says. “Tell him to take one drop of Alphagan and it may just constrict his pupil enough that it takes away some of the night-vision symptoms.”
Very diluted pilocarpine could also produce the pupil-constricting effect, Dr. Krueger notes, though it can also cause problems such as brow ache.
Even so, night-vision issues have improved significantly, Dr. Terry points out. He attributes this to the “better-every-thing factor.” The broad-beam lasers of the past did not provide as accurate an ablation zone as lasers do now, and eye tracking “has helped dramatically in getting better centered ablation. And ablation profiles have improved with the blending effects we've had from lasers,” he says.
Better patient selection and alternate technologies have also played a role. Refractive surgeons now know that performing a 13 D myopic ablation will almost certainly bring aberrations that would not occur with a 5-6 D ablation. Advances in phakic IOLs provide surgeons with a satisfactory alternative for these highly myopic patients.
■ Epithelial ingrowth. According to Dr. Holzman, corneal epithelial ingrowth is seldom a problem in primary LASIK cases, in large part due to the femtosecond laser and flap side cut architecture. “It is more likely in enhancements, especially in flap lifts of previously created micokeratome-based flaps,” Dr. Holzman explains.
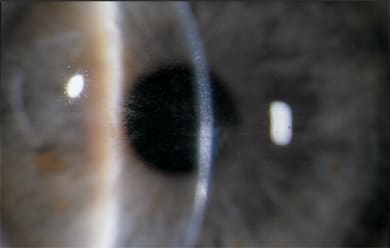
IMAGE COURTESY OF GITANE PATEL, MD, AND JAY PEPOSE, MD.
Patient one day post LASIK presented with pain, decreased vision and focal clustered infiltrates, some extending beyond the flap margin. These are warning signs of early LASIK-associated microbial keratitis, requiring flap lift, culture and scraping, antibiotic irrigation of the interface and intensive antibiotic therapy.
Ectasia — Still the Wild Card
The ultimate complication that remains, and that is sight-threatening is, of course, ectasia. “It is the one that scares physicians the most,” Dr. Krueger concedes. “If you get an ectasia, you think, what am I going to do now? Now the patient has an unstable cornea, and in the worst-case scenario, he'll need a corneal transplant to fix it.”
And while collagen cross-linking has real potential to help patients who develop ectasia after LASIK, it's still not FDA approved in the United States.“Thus, it is critical that the surgeon be extremely careful to screen out the potential risk for ectasia before surgery,” Dr. Krueger explains. “And that's just making sure there is no subclinical keratoconus to start with. Sometimes it's missed.”
Heading Off Bad Publicity
Should a complication occur, you can help avoid feeding the bad publicity beast by being honest and hands-on with patients. That starts with detailed preop discussions about the risks and benefits of refractive surgery. Dr. Schallhorn presents inflammation, dry eye and nighttime visual phenomena as possible side effects that usually resolve over time in the vast majority of patients. However, he also cautions them that some patients can have more prolonged and severe problems, and that further treatment may be necessary.
Dr. Holzman encourages developing a rapport with patients. “This shouldn't be hard, but it can be for many physicians,” he notes. “We want patients to relax during the surgery — a patient who trusts you is much more likely to relax during your surgery and be understanding with a less-than-expected result should something rare occur.”
These surgeons find, however, that most prospective patients come to their practices well educated about refractive surgery and with a realistic sense of the risks. They are generally not unduly worried about LASIK horror stories in the media.
“I think most people appreciate that there are risks with any procedure, including LASIK,” Dr. Schallhorn says. “They also appreciated that when an unhappy patient is given a voice, such as the Internet, it can appear to be a bigger problem than it is.”
Thankfully, many surgeons point out, nearly every prospective patient these days knows someone who has had refractive surgery and been delighted with the improved quality of life it has afforded them.
As for that FDA study in the works on LASIK's impact on patients' quality of life, these experts welcome it.
“I think that the FDA is trying to gather objective evidence of the results of this procedure, and that's entirely appropriate to do. It's difficult and confusing to patients to deal with the hype of advertising, the hype of some surgeons trying to gain market share,” says Dr. Terry.
“We LASIK surgeons should encourage the media and FDA to look at our procedure again, as this time they will find a much better and safer procedure,” says Dr. Holzman. OM








