Step Up to Benchmarking
It is not as difficult or as confusing as you might think — and it's good for you.
BY RENÉ LUTHE, SENIOR ASSOCIATE EDITOR
For medical practices, financial benchmarking is a lot like exercise — everyone knows that it is important for maintaining good health and that they really should make time for it — but somehow, they don't. And one reason practices give for nonexistent or irregular benchmarking isn't all that different from the one those low on willpower give for avoiding the gym: they're too busy making a living.
Other reasons, however, reflect practices' real confusion over the process of benchmarking. Many practice managers are not sure which financial statistics are important, they might not know how to collect and separate their data, and they don't always know how to maximize the value of benchmarking once they have done it.
Others trace their confusion to a changing practice environment. “What are the norms in our current state of the economy and reimbursements?” asks Richard J. Ruckman, MD, of Lufkin, Texas. “I feel that many of the traditional benchmarking ratios are no longer valid. I don't know where I should be except that I am still profitable in both my ASC and clinic. Having said that, my profit margin is definitely down from years ago, but then so are my reimbursements.”
In this article, Ophthalmology Management solicits experts' opinions on how financial benchmarking can improve your practice's health and looks at some new resources to make the process easier.
Worth the Effort
Veteran practice management consultant John Pinto reports that physicians are generally slow to grasp the value of benchmarking for the practice/business. However, he feels it's just as important, and directly comparable, to clinical benchmarking. Imagine treating a glaucoma patient without baseline data on IOP, visual fields and optic nerve. Lacking any sense of where the patient began would make it exceedingly difficult to craft a treatment plan and measure progress toward the goal. So, too, with financial benchmarking.

“Happily, the math is not that difficult, so even math-o-phobes can rapidly ascertain their key performance benchmarks and start the process at a basic level,” Mr. Pinto assures. Digging deeper into your practice's data may require the support of your accountant or a consultant. But no matter how you choose to become more fluent in benchmarking, Mr. Pinto urges practices to get busy with it pronto. “The tougher practice environment that's just around the corner demands more objective measurements,” he says.
Clearing up the Comfusion
Maureen Waddle, senior consultant at BSM Consulting and co-author of a human resources column for Administrative Eye Care, finds that practices typically have some misconceptions about benchmarking that are holding them back. “There is a lack of understanding about where the numbers come from or what influences the numbers, and therefore practices aren't making good business decisions about what to do with them,” she says.
Another common error Ms. Waddle encounters is that practices learn of some national benchmark that has been published and panic if they don't fall within the cited range, or make a business decision based solely on that published benchmark. “Yet they really don't even know why their practice falls outside of the benchmark, and if that's even a bad thing,” Ms. Waddle explains. “That's always the biggest challenge.”
An incomplete understanding regarding the definitions used in practice benchmarking is another typical obstacle to ascertaining accurate, helpful data. In presentations conducted at meetings such as the American Academy of Ophthalmology's 2009 annual meeting in San Francisco, Ms. Waddle reported that she is frequently asked what should be included under definitions of various expenses. According to her, an uncertain grasp of these definitions leads many practices to fail to “back out” some of their physicians' expenses or employed doctors from their overhead. “They then wonder why their overhead, their staffing ratios, are too high compared to the national benchmarks,” she says.
She finds this particularly true of solo practices. As small businesses, it is crucial that they focus on the definitions involved in choosing their data and be careful to back out many of their doctor-related expenses before they compare their overhead ratios to national averages.
A new benchmarking database from the AAO, she believes, will go a long way toward establishing uniform definitions for practices (see sidebar).
Where to Start?
As for which benchmarks to measure, Ms. Waddle says that she typically tells practices to start at the top. “That's revenue,” she says. Measuring revenue generated entails looking at revenue per full-time equivalent (FTE), revenue per office visits and then looking at operating expense.
“How much does it cost you per dollar that comes in to get that dollar?” Ms. Waddle asks.
Then comes staffing. “Always the biggest expense that a practice has,” she says. Moreover, there are three key ratios related to staffing:
► The staffing/expense ratio.
► Revenue per FTE staff member. Typically, this runs around $140,000 per FTE equivalent. However, Waddle explains, “If you're a high-volume surgical practice and have a lot of staff, and yet you're able to generate $200,000 per staff member, your FTE staff members count might be out of line; however, you're doing just fine.”
Mr. Pinto identifies approximately 50 benchmarks and norms for practices to track.
“That sounds daunting,” he allows, “until you remember that an internist has to memorize thousands of norms. In this context, becoming your practice's resident business ‘doctor’ is not so much of a chore.”
According to Mr. Pinto, what should be key drivers for every eyecare practice include:
► Profit margin.► Revenue growth rate.
► Total and established patient growth rate.
► Average revenue per patient visit.
► Surgical density.
► Optical sales per patient visit.
► Cost margins for staff, facilities and marketing.
Additionally, says Mr. Pinto, every management consultant has his or her own proprietary set of benchmarks. “These are updated regularly and indexed to such variables as practice scale, subspecialty interest and location.”
When it comes to rents, Ms. Waddle says that rent expense ratios tend to run the same for most industries: 7% to 8% of revenue. “So I don't typically pay attention to that unless we're doing a feasibility analysis as to whether to open up a new office or to build out a new office,” she explains.
Benchmarking Reimbursements
Attempting to benchmark reimbursement rates from third-party payers can be particularly frustrating for practices because so much is out of your control — the rate of reimbursement itself, as well as the speed of remittance. But new resources can help practices not only hasten the process but show them valuable data about themselves.
Medical billing clearinghouses help practices track claims and payments. One, Navicure, offers a visual, Web-based presentation in real time to show practices where their claims are in the process, why a given claim was rejected and to head off rejections by flagging mistakes. According to Navicure vice president Ken Bradley, practices frequently come to Navicure because they are concerned about not meeting a benchmark for collections. Internal studies, he says, shows that the company can reduce the number of rejections and denials by 50%, as well as significantly reduce the number of days a claim spends in AR.
“Part of the problem is that every payer is so different,” explains Mr. Bradley. “Medicare is different from Blue Shield, which is different from Medicaid.”
Navicure's medical billing clearinghouse simplifies the billing process to six different “boxes” showing what stage the individual claims are in and what their status is. The company gathers response data from the many payers involved, standardizes it and links it to the original claim.
A claims “scoreboard” shows which the payer has rejected, and drill-down capacity allows the practice to learn the reason why. Practices have the option of correcting the claim online.
In addition to a less stressful billing process, the result, says Mr. Bradley, is a more defined, strategic goal-setting ability for the practice.
“They can start setting measures,” he explains. “Until you can measure those claims, until you can see those in a form that has been summarized and standardized, it's hard to really set measures and be able run the practice with goals and strategic objectives to be met.”
To further help practices strategize, the company has added time dimensions to all their scoreboards. Practices can check on their numbers for the previous week, month or year. “They can see what their top 10 rejected claims were and how that trends by physician or by user within the practice,” Mr. Bradley says. Armed with the knowledge of what their top rejections are, the practice can then examine ways to prevent them.
| AAO Initiative Aims to Standardize and Improve Benchmarking |
|---|
In an effort to help both itself and its members promote the health of eyecare practices in the United States today, the American Academy of Ophthalmology has in recent years started asking for benchmarking data annually from its members. The Web-based survey and resulting database grew out of a task force that was trying to ascertain the most efficient practice model. “Our task force looked at a number of models and what they concluded is that you really cannot say there is one ideal practice model,” says Donna Lock. The AAO began collecting the data in 2007. In order to offer a detailed, apples-to-apples comparison of benchmarks, the AAO's survey includes a number of filters. Participants are asked to enter the number of physicians, the number of MDs and ODs, subspecialty, region, metropolitan area, facility type, total clinical operating expenses, total number of FTE front-office staff, total billing staff wage and benefit cost as a percentage of net collections, among many other figures (see full list at right). The AAO offers definitions for each measure, as well as a guide to interpreting the benchmarks. “There needs to be a minimum of 15 like entries for them to make these comparisons,” explains Ms. Lock. The survey offers the flexibility to pull benchmarking data on a number of subsets “So a solo practice could compare itself to other solo practices, or a three-doctor retinal practice in the Pacific Northwest to other three-doctor retinal practices in the Pacific Northwest.” Only AAO members are permitted to participate in the survey or to have access to the online reporting. Ms. Lock says that the AAOE tries to keep the survey relatively short. “We didn't want it to be so time-consuming as to be a deterrent in terms of participation.” Practices enter up to 36 data elements and receive 43 benchmarks. Ms. Lock reports that it typically takes practices two to four hours to collect and enter the data. “Once you find out what information you need to collect and how you need to separate your information, it becomes easier,” she says. Practices are rewarded for their time and effort with a comprehensive, very detailed list of measurements. The AAOE begins collecting data for 2009 in February. For more information, go to www.aao.org/benchmarking. |
|
Benchmarks Collected in the AAO's Database: Professional clinical collections per FTE ophthalmologist Professional clinical collections per FTE optometrist Clinical revenue per encounter for ophthalmologist Clinical revenue per encounter for optometrist Practice net collections per FTE staff member Practice net collections per FTE billing office staffer Clinic operating expenses per encounter by entire practice Clinical operating expenses as % of net collections Non MD/DO/OD clinical staff cost per encounter Front office staff cost per encounter Total staff wage and benefit cost as % of net collections Total front office wage & benefit cost as % of net collections Total billing staff wage & benefit cost as % of net collections Total Non-MD/DO/OD clinical staff wage and benefit costs as % of net collections Number FTE optometrists per FTE ophthalmologist Number FTE front office staff per FTE MD/DO/OD Number FTE non-MD/DO/OD clinical staff per FTE MD/DO/OD Total days clinical A/R outstanding Percentage clinical A/R in “Current” Percentage clinical A/R in “31-60 days” Percentage clinical A/R in “61-90 days” Percentage clinical A/R in “91-120 days” Percentage clinical A/R in “121+ days” Total encounters per FTE ophthalmologist Total encounters per FTE optometrist New patient encounters as % of total practice encounters Encounters per FTE Non-MD/DO/OD clinical staff Encounters per FTE Front office staff Total clinic facility expenses as % of total net collections Net clinical compensation per FTE ophthalmologist Net clinical compensation per FTE optometrist Net clinical compensation per FTE owner Optical collections per FTE MD/DO/OD Optical collections per FTE Optician Optical collections per practice encounter Optical cost of goods sold as % of net optical collections Optical operating expenses as % of net optical collections Optical Rx capture rate (not all practices capture refractions in the same manner) Average revenue per sale Average cost per sale Average net profit per sale Total optical net profit or loss Percentage of practices that employ ODs |
Just Do It
Ms. Waddle urges practices to remember that benchmarking is not about meeting a national standard. Keeping in mind your practice's various contexts — region, specialty, number of doctors, etc. — is very important to gauging your health.
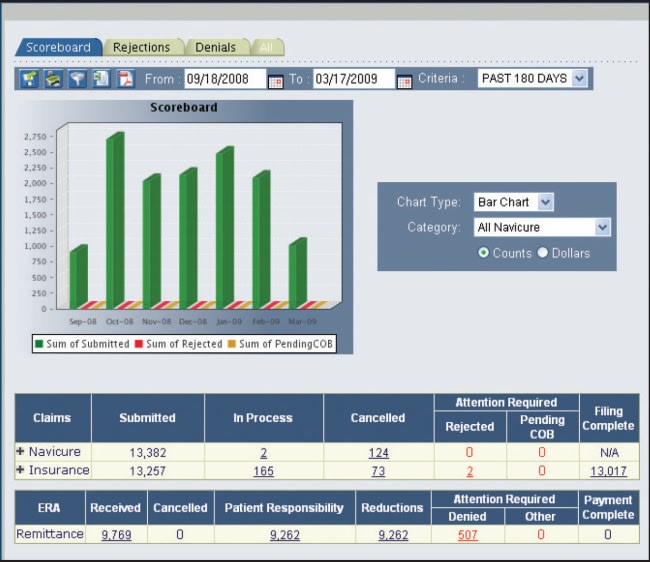
Navicure's Web-based tracking software provides up to date status on submitted claims.
“If you're in a more urban area — San Francisco or Los Angeles or New York — your staff expenses are, just by the nature of the beast, going to be above the national averages,” she says. The competitiveness of your region's job market and the availability of people in that marketplace, are going to influence that type of ratio as well.
The important thing, she says, is that practices do measure their data. “Call it benchmarking, call it whatever you want — it is key that practices have consistent measures, and that they are comparing against themselves first and foremost,” says Ms. Waddle.
Next is formulating a plan based on those measurements. The biggest mistake, according to her, is that practices fail to do this.
More often, she says, practices take a sporadic approach to benchmarking. “They do it once and maybe they make some decisions based on that, but there's no continuous improvement plan,” Ms. Waddle explains. Practices need to continue to measure on a regular basis and base decisions on the information. “They shouldn't make a knee-jerk decision just because they ran a benchmark once, compared that to a national benchmark, and didn't like how it looked.”
Mr. Pinto agrees that regular benchmarking needs to be a priority with every healthcare practice.
“Four hundred years ago, European doctors had just one lab test: tasting their sick patient's urine,” he says. “Today, modern doctors have thousands of tests — all of which are more pleasant to administer! However, modern managers are only just catching up. “Business benchmarks are the essential lab tests of a practice's financial and volumetric health. To omit these from your management toolbox is like practicing medieval medicine in the 21st century.” OM








