Putting the Squeeze on OCT Fees
Will reimbursement cuts blunt the growth of this versatile technology?
By Samantha Stahl, Assistant Editor
These days, reports of a new reimbursement cut are as common as reports on the lackluster economy. As healthcare reform pursues “affordability,” physicians know all too well that policy-makers rarely have their best interests at heart.
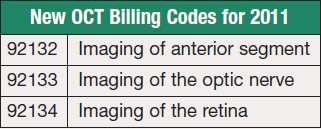
The latest victim of the cost-cutting sword? Optical coherence tomography. Ophthalmic coding expert Riva Lee Asbell of Fort Lauderdale explains that beginning January 1, the former OCT billing code, 92135, will be eliminated completely and replaced by three new codes: 92132 for imaging of the anterior segment, 92133 for the optic nerve and 92134 for the retina. The bad news: all OCT codes are now considered “unilateral or bilateral” — no more separate billing of each eye for bilateral use. Additionally, retina and optic nerve scanning codes cannot be reported together.
As if to rub salt in the wound, the payment for OCT has also been decreased. William Rich, MD, medical director of health policy for the AAO, reports that the average payment for code 92135 in 2010 was $52.45. The payment for the new codes will be $48.33, a decline of about 8%. For those who are accustomed to reporting the code twice for bilateral use, this amounts to a 54% cut.
OCT technology has rapidly evolved in recent years, introducing spectral domain OCT and a battery of new uses. As the devices became more sophisticated and physicians recognized new diagnostic opportunities, OCT usage shot up — attracting the attention of bean-counters. So why can't a technology this promising be left alone?
“The code came up for re-evaluation because it was one of the three fastest growing codes in Medicare. Economists assume if something grows rapidly in volume there may be overvaluation,” says Dr. Rich. “The old physician survey of time needed to provide the service was 26 minutes! Obviously the new survey showed substantially less time so, unfortunately, OCT was reassessed at a lower value.” Nevertheless, his advice for how to cope with the cut is simple: “Go about your business.”
The Business Side
In a typical general ophthalmology practice, OCT tests are used in around 3% to 12% of total visits, says practice management consultant John Pinto, meaning approximately 450 tests for a doctor who sees 6,000 patients per year. This translates to around $20,000 in annual gross revenue per physician. Group practices, naturally, derive exponentially more revenue from an OCT scanner.
Watching a former revenue growth area abruptly begin to decline will be a bitter pill to swallow for many. “Ad hoc, unsubstantiated cuts such as these combined with looming threats of double-digit Medicare fee reductions contribute to a profound sense of anxiety in the profession today,” Mr. Pinto says.
“A few innocent percentage points here and there are starting to add to the ‘misery index’ and are taking a toll, not only on provider morale, but on the time, cheerfulness and attention they have to give to each patient,” Mr Pinto says. “We have all clearly entered a ‘stiff upper lip’ era in ambulatory health care.”
While physicians whose use of OCT is primarily unilateral won't have to take a huge hit to their finances, others doing a substantial amount of bilateral scans (glaucoma specialists, for instance) must prepare to re-evaluate. While no one is suggesting that a cheaper machine could or should replace OCT — the technology has become too crucial to go by the wayside — many are saying that there's no time like the present to pay close attention to practice finances.
“Control costs and make sure you aren't missing legitimate charges,” says coding and practice management consultant Sue Corcoran of California. She also says that a number of practices are postponing purchases of OCT devices.
Michael Ober, MD, a retina specialist from Southfield, Mich., concurs. “If considering a new purchase, go through a detailed financial plan to estimate usage, cost, personnel, etc., and weigh against reimbursement to calculate whether a purchase is going to gain or lose money for the practice. There are still times when a contact lens macular exam gives more information than the best OCT on the market.”
Though some generalists and subspecialties can get by with OCT alternatives, he says that the retina community has found OCT to be an indispensable tool. He doesn't foresee reimbursement cuts changing the frequency in which the technology is used, but it will cause a major pause before any additional OCT investment. The retina community's recent collective upgrade from time domain to spectral domain was made possible by the former reimbursement rates, Dr. Ober says. Nowadays, however, “we will see a reduction in our bottom line and a hesitancy to purchase OCTs until office efficiency makes it absolutely necessary.”
“Those practices where OCT is not essential will certainly reconsider a pending new purchase, since the reduced reimbursement signifies a greater time for a new machine to cover its expenses,” he says. For practices that already own a machine, he advises that they continue to use OCT when clinically indicated, since reducing use would only make the device relatively more expensive.
His biggest fear, he says, is that slashed reimbursement and subsequently reduced demand for new purchases will discourage manufacturers from continuing to develop technology for improved resolution and adding new software features. “Manufacturers have produced significant technological innovation with respect to OCT in the past 10 years that has been driven by a demand for their product. The impending reduction in demand will likely reduce their budget for research and innovation.”
Michael Repka, MD, of Baltimore, recommends that worried practices should “make sure they have the volume of studies to support the investment [of a new OCT] or share with another practice.” The Medicare system pays primarily for physician work, he explains. “Technology in general does not involve as much physician work as older techniques,” he says. “It increases the physician's efficiency, but the decreasing work will lead to lower payments.
Thus, doctors find themselves in an ironic predicament: as it becomes possible to provide quicker, better outcomes for patients, their financial reward decreases.
| Ready to Invest In OCT? Questions to Ask Before You Buy |
|---|
|
► Does this machine need to be portable so it can be used in multiple exam rooms/practices? ► How much will the labor cost for this machine be? ► What does a pro-forma return on investment calculation say a new machine can cost without limiting profitability? ► Does SD-OCT provide needed features that TD-OCT can't offer? ► Will a multi-purpose machine cause a bottleneck at the station and hurt business flow? |
The Technical Side
Aside from lower reimbursements, what other constraints can physicians look forward to? Some doctors worry that fee cuts will ultimately mean a huge compromise in technology developments. There is some concern that instrument manufacturers will likely focus on efficiency more so than major technical breakthroughs, slowing the consistent pace of improvements to which the ophthalmic world has grown warmly accustomed.
Efficiency will indeed have to be a key component of current and future OCT device buying decisions, says Marianne Whitby, senior marketing manager at Carl Zeiss Meditec. “Healthcare demographics, in particular the aging population and the availability of new therapies, will require doctors to see more patients in less time. Instruments and workflow solutions which are efficient and easy to use will be advantageous to all practices,” she says. Marketing strategies from industry to physicians have no need to change, she says, since the technology has proven itself within the eyecare field.
Ms. Whitby is confident that the associated return on Zeiss's OCT product portfolio justifies the purchase of a new machine. Lower cost SD-OCT machines, like Zeiss's Cirrus Model 400, aim to make it possible for budget-conscious practices to incorporate the technology into their office repertoire without investing a large sum. For those who are concerned about investing in capital equipment right now, given the state of the economy and the uncertainty about healthcare reform's impact, manufacturers are sensitive to such concerns and are looking for cost-effective solutions.
Pravin Dugel, MD, a retina specialist from Phoenix, encourages practices to arm themselves with a realistic sense of profitability before any purchases. “Sales people are going to say, ‘Divide the cost of the machine by the number of times you do the procedure. After 50 uses you've already paid for it.’” He says that staff time and other direct costs to run OCT need to be considered to calculate pure profit.
Dr. Dugel says that practices should go through a checklist as they decide what they need in their OCT machine. One of the first questions to ask is who will use the machine. “Is it for a single-subspecialty, multi-specialty or general practice? In a multi-specialty practice, the algorithm changes completely. What can all of the doctors be happy with?”
Despite a dramatic turn towards SD-OCT, Dr. Dugel contends that, for many ophthalmologists, time domain can get the job done. “All research trials demand time-domain OCT because new ones don't have universal calibration. In a pure retina practice, you can diagnose the vast majority with time domain,” he says. “The imaging is better in newer generation machines, but how do you justify the additional cost?”
Considerable competition in the OCT market has caused some downward pressure on pricing, according to Bob Gibson, vice president of marketing at Topcon. He worries, however, that the reimbursement cut will make it difficult for more advanced machines to catch on in the US. Companies with a global presence, such as Topcon, can benefit from international sales where reimbursement cuts are less of an issue. Perhaps success overseas might enable companies to maintain their product development efforts, and ultimately US physicians will benefit as well.
Mr. Gibson predicts that the reimbursement cut will slow down the adoption of the technology primarily for optometrists, general ophthalmologists and refractive surgeons. “However, I think physicians who have invested in a new OCT will continue to use it. Retina and glaucoma specialists will continue to use OCT as an aide in the diagnosis and monitoring of disease,” he says.
Much of Topcon's product development, Mr. Gibson says, has focused on multi-function instruments that offer more opportunities for practices to recoup their investment. Systems that incorporate OCT and a variety of fundus imaging techniques, like color photography, fluorescein angiography and autofluorescence, offer greater versatility to physicians.
While Dr. Dugel agrees that multi-use instruments can be a smart investment, he recommends making sure you need the additional capabilities before shelling out for an expensive machine. “You need to ask, what do I really want to use this for? Do I need autofluorescence? CT angiography? Are those things important to me? And how does that influence your business flow — will there be a bottleneck at one station?”
For smaller offices, making a large equipment purchase may simply be impossible. “The current economy and continuing Medicare reimbursement scrutiny are pushing clinicians to be more conservative in their capital equipment purchases,” says Jay Wei, CEO and founder of Optovue. “One of the options is the sharing of devices over multiple offices or practice locations, and a smaller, portable OCT is a perfect fit for this scenario.” The iVue, Optovue's compact iVue SD-OCT, offers clinicians the option of purchasing one versus multiple systems, he says, providing an opportunity to conserve capital.
Looking to the Future
Though taking a harder look at practice finances is an indisputable must, most of the future implications of the OCT reimbursement cut are still up in the air. The ophthalmology community can only hope that the technology's development continues on the same steady path it has traveled over the past few years.
Dr. Dugel says, “The unfortunate part of this is that when we show we're doing things better and the more efficiently we can deliver healthcare, we get punished on the reimbursement end. The more we do, the more we get punished.” OM








