Improve Your Optic Nerve Evaluation
Here's a systematic approach for performing a thorough glaucoma evaluation.
BY JODY PILTZ-SEYMOUR, MD
As other glaucoma specialists have noted, performing an optic nerve evaluation seems to be something of a vanishing art, as clinicians have become perhaps a little too accustomed to relying on the latest diagnostic equipment, such as HRT. But comprehensive ophthalmologists are on the front lines of glaucoma detection, and as we all know, this is a disease that is asymptomatic until significant, irreversible vision loss has occurred. Clinicians cannot depend on equipment alone.
In this article, I'll outline a straightforward routine for performing a thorough optic nerve exam in your office. Remember, nothing is as important as what you can see with your own eyes while it is right there in front of you.
Getting a Good View
Most optic nerve exams are done with handheld lenses. For those first learning to perform the exam, I recommend using a 78-diopter lens — which provides a nice balance between magnification and field of view — and dilating the pupil as widely if possible. A superfield lens by Volk, Inc. can provide excellent viewing through most undilated pupils, but it is important to keep the light parallel with the visual axis and to lower the intensity of the light source. Additionally, fundus contact lenses can be helpful to examine optic nerves that are difficult to evaluate, particularly if the ocular surface is dry or irregular, providing better clarity and stereopsis. The direct ophthalmoscope can provide a monoscopic view of the disc.
In order to properly visualize the optic nerve, it is important to have the patient fixate exactly where you want — otherwise, you will never find what you're looking for. When using fundus lenses, the patient should fixate slightly nasally. This is best achieved by asking them to look at your opposite ear. When using the direct ophthalmoscope, ask the patient to look straight ahead and a little bit upward.
It is important to stress that the examination of the optic nerve is a dynamic process. If you take your ophthalmoscope beam or slit lamp beam and pass it over the optic nerve, you can actually see how the light plays off the nerve tissue. With a static light you may not see the contour changes or even the quality of the neuroretinal rim, but by moving the light across the disc, sometimes the rim can appear “moth-eaten.” The rim tissue is present but not dense and the light appears to shine through it.
Once you have obtained a good view of the optic nerve, you can begin your examination.
#1 Identify the Edge of the Optic Disc and Determine Disc Size
■ Find the edge. The most basic thing we must identify first is the edge of the disc. It is vitally important but sometimes challenging because peripapillary changes around the optic nerve can mimic rim, as can the scleral insertion of the optic nerve. In fact, this is one of the first things that often fools clinicians. You have to be able to really identify where the edge of the disc rim is and distinguish it from the scleral insertion and peripapillary changes.
■ Size matters. There is great deal of anatomical varia tion in the size of the optic disc among the population, so what constitutes a “normal” appearance is highly patient-specific. Figure 1 shows two different, normal optic nerves. The one on the left is small and has almost no cup in the center, and disc on the right is large with a correspondingly large cup. While they look very different, they illustrate the range of physiologic disc appearances.

Figure 1. The size of the cup should be proportional to the optic nerve. On the left is a small optic nerve with almost no cup; on the right, a large cup in a large nerve. ALL IMAGES COURTESY OF JODY PILTZ-SEYMOUR, MD
■ Measurement tips. Since the size of the cup of the optic nerve is directly related to the size of the disc, the first step in interpreting the significance of the size of the cup and the cup-to-disc ratio is determining the size of the optic disc. As for techniques to measure disc size, I usually use the direct ophthalmoscope. If you use the 5-degree spot, which is the middle spot size on the Haag-Streit ophthalmoscope, it shines a circle of constant size on the retina of patients with refractive errors within the range of +8 diopters to −8 diopters. You can use this spot to measure the size of the optic nerve. An average-sized optic nerve should be slightly larger than the spot, with the edges of the disc just peeking out around the light when it is placed over the disc. If the spot of light is the same size or smaller, then it is a small optic nerve. If the optic disc is much larger than the spot, then you know it is big.
There is another way to measure disc size using your fundus lens. You dial the height of the light beam to match the height of the optic nerve and then read the number off of the scale on the slit lamp. These measurements vary depending of the power of the fundus lens that used; for the 90-diopter lens, an average optic nerve will measure 1.4, the disc is large if the light beam is more than 1.6 and the disc is small if it is less than 1.2. Using the light beam is also an excellent way of looking for disc asymmetry by checking for relative differences between the height of the light beam in the two eyes.
About the Cup-Disc Ratio
While the cup-to-disc ratio is often talked about, in my experience it really is not that clinically useful in direct patient care. It is very poorly reproducible between observers and does not tell you enough about the quality of the disc such as the shape of the disc, the quality of the rim, and whether there is notching or generalized loss. But a picture is worth a thousand words; it is so much more valuable to draw and/or photograph what you see.
I strongly recommend both drawing and photographing the disc. When you draw the optic nerve, it forces you to closely scrutinize the contour of the disc. A photograph is invaluable for future comparisons, but if a drawing is not done, the clinician may not spend the time needed to really see all the disc has to offer. The more you look, the more you will see. Optic nerve evaluation is the single most important part of the glaucoma clinical examination, so spending a few extra moments can provide great insights into the nature of your patient's glaucomatous process.
One of the most important things — taught to me the first day of my fellowship — was the importance of really knowing how big a disc is before you worry about anything else. Because if you don't, you're going to miss the diagnosis of glaucoma in eyes with small optic discs and over-diagnose glaucoma in large optic nerves. Just remember that the size of the optic nerve is going to determine the significance of whatever disc appearance you're seeing. You can expect to see a smaller-than-average cup in a small optic nerve and a larger-than-average cup in a larger optic nerve. So, if an optic disc is very small, a cup-to-disc ratio of 0.4 may be pathologic, and in a larger disc, a cup-to-disc ratio of 0.8 may be absolutely normal.
#2 Identify the Rim Edge And Evaluate the Rim Tissue
While people often refer to the appearance of the cup in glaucoma, the cup itself is not very important and is mainly useful only for determining the edge of the disc rim. The disc rim is what is really important, because that is where the nerve tissue is. Check whether there is viable, healthy rim tissue between the edge of the disc and the edge of the cup. With glaucoma, you really are looking for contour changes, not just color differences. That's why we identify the edge of the optic disc and then the edge of the disc rim.
The “ISNT rule” helps you evaluate the rim by highlighting the normal appearance of rim thickness. In the average healthy optic nerve, the neuroretinal rim is thickest Inferiorly, then Superiorly, then Nasally and finally Temporally. ISNT helps you know if the optic nerve you are looking at is typical. The rim should be “juiciest” inferiorly and superiorly where the arcuate bundles converge on the optic nerve. The inferior and superior rims are preferentially damaged in glaucoma should be closely examined for thinning and notching.
Patterns of Damage
Optic nerves can develop glaucoma in many different ways. Concentric cupping is a common pattern of glaucomatous damage (Figure 2) where the optic nerve loses just some rim tissue everywhere. Very often this kind of disc damage occurs in eyes with high intraocular pressure and yet since the damage is diffuse, the visual fields can remain normal despite significant rim loss. There is extensive literature, particularly described by Quigley, demonstrating that you can lose up to half the optic nerve axons before you see a visual field defect, and that is particularly true with concentric cupping.

Figure 2. Concentric cupping, a common pattern of glaucomatous damage.
Why is the possible? The patient is losing all reserve tissue everywhere, but no single region becomes 100% depleted. There is quite a bit of redundancy in optic nerve tissue. To illustrate the point, let's say that there are five axons serving the same area of the retina. The patient can lose one, two, three and even four axons but may still have relatively normal nerve function at that location. With concentric loss, as long as the patient does not lose that fifth axon, function can remain relatively stable. That's why with this kind of glaucoma the extent of nerve damage can be substantial before it manifests in visual field loss. However, once the reserve is depleted, functional loss progresses quickly with rapid development and progression of visual field damage.
Focal loss, on the other hand, will cause a visual field defect much earlier, because while most of the patient's nerve may be generally healthy, there is a “bite” out of the rim in one spot, Patients with this type of glaucoma develop focal arcuate visual field damage earlier in the course of their disease, often associated with optic disc hemorrhages. It is common for glaucoma damage to present with a mix of generalized and focal loss (Figure 3).

Figure 3. Glaucomatous damage frequently presents with a mix of generalized and focal loss.
Another form of glaucomatous damage, called senile sclerotic (Figure 4), presents with saucerization and peripapillary atrophy and is often seen in more elderly patients with vascular disease. Senile sclerotic damage is also the form of cupping associated with the moth-eaten rim appearance. It is the kind of disc where one physician looks at it and says, “That's a 0.3 cup-disc ratio,” and the next physician looks at it and says, “That's a 0.9 cup-disc ratio,” because there is gentle sloping of the rim, and the rim tissue that is present often seems to disappear when you move the light across it. That's why it is always important to shine your light and move it across the surface of the disc.

Figure 4. Senile sclerotic disccupping is associated with a “moth-eaten” rim appearance.
Now for a word of warning about your myopic patients: They have very difficult discs to interpret. Often these discs are tilted, misshapen and just difficult to follow They may have crescents that look like peripapillary changes and associated congenital visual field defects.
While the conventional wisdom states that glaucoma does not cause pallor, pallor without rim contour changes may develop after an acute transient spike of IOP. Typical situations to see pallor are after acute angle-closure glaucoma, after a postoperative surgical IOP spike or any other acute glaucoma with highly elevated pressure. However, if you see pallor, you must rule out other types of optic nerve disease.
Asymmetric cupping of more than 0.2 between the two eyes should raise suspicion of possible glaucomatous rim loss. The first thing I do when I see someone with asymmetry is check for corresponding asymmetry of the size or shape of the optic disc. While most people have symmetric sized discs, not everyone has read the rulebook! Some people have congenital asymmetry of the disc size or even differently shaped optic nerves. If one optic nerve is oval and one is round, there will always be an asymmetric appearance even if the rim tissue is normal in both eyes. However, glaucoma typically develops asymmetrically, so asymmetric rim loss may be an early sign of glaucoma damage. It is always important to look for optic nerve asymmetry between the two eyes, but first make sure that there is not disc asymmetry.
#3 Don't Forget Hemorrhages
Disc hemorrhages are a warning sign that an eye is at risk of developing glaucoma or that manifest glaucoma may be progressing. Because they are subtle and may masquerade as small blood vessels, the majority of disc hemorrhages will be missed unless you actively look for them, so please be sure to do so. In fact, when I am looking at the disc, after I evaluate the health of the rim, I say to myself, “And now I'm going to look for disc hemorrhages!” It's a conscious step for me to check off.
Disc hemorrhages look like little blood vessels as they cross the disc, but they do not continue on, as retinal vessels would. Optic disc hemorrhages may be quite subtle, as seen in Figure 5. They are transient but often recur. They develop most commonly at the inferior followed by superior rims. Focal notching may develop in the location of a prior hemorrhage, and future hemorrhages occur at the edge of rim notches.

Figure 5. Optic dischemorrhages are transient and may recur.
For years, disc hemorrhages weren't even recognized. They had been described in the literature by Bjerrun in 1889, but were not given clinical significance until they were reintroduced by Drance and Begg in 1970. People had been looking at optic nerves all those years, but did not consciously recognize the hemorrhages. This reminds us to make a concerted effort to actively look for hemorrhages.
#4 Peripapillary Changes
Now it's time to check for the peripapillary changes around the optic nerve. There are two types of peripapillary changes, zone alpha and zone beta. Alpha atrophy is a region of irregular pigmentation of the retinal pigment epithelium. It is a normal finding and is not associated with glaucoma damage. More important for glaucoma is beta peripapillary atrophy, which results from atrophy of both the RPE and choriocapillaris, leaving a crescent-like region adjacent to the disc where the sclera and larger choroidal vessels can be seen.
Beta atrophy can develop in one region of the disc edge or can extend around the entire disc circumference. It is preferentially located at the disc edge corresponding to areas of neuroretinal rim and nerve fiber layer loss. It is often seen as a first sign of glaucoma damage in small optic nerves with corresponding small cups where early neuroretinal rim loss may be difficult to determine. While beta zone atrophy is more common in eyes with glaucoma, it is not pathognomonic for glaucoma damage and can be seen in other optic neuropathies. (Figure 6).
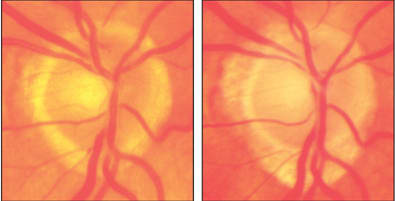
Figure 6. Look for changes in the peripapillary area over time. On the left, the patient's optic nerve in 1988; on the right, in 1995.
#5 Look at the RNFL
This one is sort of a bonus, because I find that most comprehensive ophthalmologists don't examine the retinal nerve fiber layer. This is probably because it is fairly difficult to see with your own eyes; it is much easier to see with a photograph. The good news is that you don't always need fancy, state-of-the-art equipment for such photos — a fundus camera will do the job. And while it is easier to see on red-free photos, many nerve fiber defects can be seen on magnified digital color photos, particularly in more darkly pigmented patients.
However, you can see the RNFL without taking a photo — looking in stereo is helpful, as is viewing under magnification with a red-free (green) light.
In a healthy RNFL, you will see striations on the retinal surface that blur the fine retinal vessels. The fibers are thickest in the arcuate bundles and these regions reflect light more creating a light-dark-light pattern; normally, there is a bright reflex over the superior arcuate fibers, a darker region across the macula and then bright again over the inferior arcuate bundles. Loss of this pattern or greater visibility and clarity of the fine retinal vessels indicate loss of the surface retinal nerve fibers. Diffuse loss causes a more “ground glass” appearance with loss of striations, while focal loss is more easily detected as a distinct dark arc where the nerve fibers are absent. Figure 7 shows signs of early loss.

Figure 7. Early loss of the retinal nerve fiber layer is shown at left, with the corresponding optic nerve head image at right.
So, the Take-home Message is…
Look, look, look! The optic nerve can provide a plethora of information about whether someone has glaucoma, the nature of the glaucoma and whether the disease is progressing. By evaluating the optic disc, you can learn so much that can greatly affect the care of your patient. Please remember to perform an optic nerve evaluation on your patients in a systematic fashion. Evaluate the size and the rim, look for hemorrhages, then evaluate the peripapillary region and the nerve fiber layer. Compare the patient's two eyes and keep in mind how disc size affects the significance of your findings. Additionally, keep in mind that you must compare the optic nerve you see in front of you today to that patient's baseline. Use stereopsis and magnification to improve observation and detect true contour changes. And remember, the more you look, the more you will see! OM

|
Jody Piltz-Seymour, MD, is an adjunct associate professor of ophthalmology with the University of Pennsylvania Health System, and in private practice in the Philadelphia area. She can be reached at jody.seymour@hotmail.com. |








