Great Debates in Refractive Surgery
A revealing look at what unites and what divides the surgical community.
By Karl G. Stonecipher, MD
Refractive surgery has been part of mainstream medicine for approximately 15 years now and, although today's procedures are superior to earlier techniques, controversies still abound. Consensus, even in a data-driven field like medicine, is always hard to come by — even among experts. That's inherently a good thing, as the community as a whole benefits from the varied opinions and expertise of its members.
I've been taking the pulse of that community each year at the American Society of Cataract and Refractive Surgery meeting by presenting a course called "Controversies in Refractive Surgery" along with my colleagues William Trattler, Steve Slade, John Doane, Steve Dell and Eric Donnenfeld. Though it's always been a revealing discussion, this year we added a realtime audience response system that allowed us to query both a panel of experts and the audience on salient topics, such as how thick the cornea should be for LASIK and use of mitomycin C — whatever we thought were the controversies du jour.
Of course, the answers of our panel and our audience did not always match up, providing for spirited, rigorous medical discussions. What we and many of our participants found so exciting was that the course allowed us to investigate what the experts view as current standard operating procedures and compare those to the perspectives of the general ophthalmologist and refractive surgeon.
In other words, it tells us who is doing what, how, when and why in both refractive and refractive-cataract surgery. I think that we refractive surgeons enjoy learning from each other and that's why this course has been popular. In this article, I will present some of our most interesting debates.
Refractive Treatments of Choice
When it comes to treating myopia, we found that LASIK is largely still king. Out of a sample size of 115, fully 86% of respondents named LASIK as their choice for correction of myopia of less than 7 D (see Figure 1). PRK was a distant second place at 10% (both LASEK and ICLs got 2% of respondents' votes).
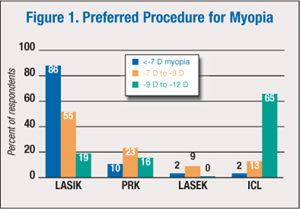
For myopia between 7 and 9 D, LASIK was still the first choice, but for only 55% of surgeons in the audience. PRK was again rated second, but now with 23% of the vote. ICLs also made substantial gains, garnering third place with 13%, while LASEK was the choice of 9% of respondents.
In considering options for high myopia (−9 to −12 D), however, ICLs leaped to the head of the pack, with 65% of respondents ranked it their treatment of choice. Especially at the −12 D range, we found it to be almost a guarantee that the surgeon would choose an ICL — 92% of respondents chose it for these patients. Meanwhile LASIK moved to second place for the −9 to −12 D range (19%), with PRK close behind for third (16%); none of the respondents chose LASEK for high myopia.
I suspect that surgeon's choice of procedure here has something to do with their laser platform. For instance, I tend to use my Wavelight in higher myopes rather than the Visx laser. A surgeon who does not have access to something like the Wavelight may choose to go with another method of refractive correction lower on the scale of myopia.
When we queried our audience about their preferences for treating hyperopia, we found LASIK again in the position of being number one — up to a point (see Figure 2). For hyperopia less than 2 D, it was the choice of 95% of surgeons. Nothing else came close, with only 3% choosing PRK as their treatment, and 2% choosing lens surgery. Similarly, for hyperopia of 2 D to 4 D, 90% chose LASIK. Lens surgery grew to 5%, PRK stayed at 3% and 2% chose LASEK.
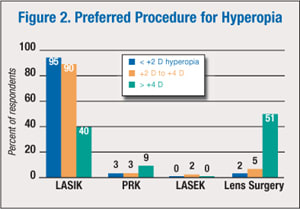
However, for hyperopia greater than 4 D, the situation changes significantly. At that level, more surgeons are going to lens surgery for hyperopia. Of course, 4 D hyperopes don't walk through the door every day, and most of those who do are older patients. More and more, I'm seeing that it is increasingly likely that +4s will get an intraocular procedure. I suspect that a lot of ophthalmologists who attend these sessions may not have access to a laser, and in that case, they are more prone to go with an intraocular procedure. They're more likely to offer the person an intraocular option if that's their comfort zone and the patient is a +6 or +7 or +8, as opposed to referring the case out to someone else.
Corneal Measurements
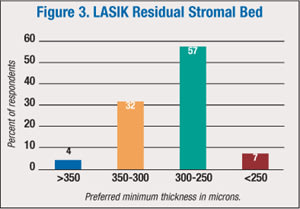
When it came to the issue of final residual stromal bed or total corneal thickness in both PRK and LASIK procedures, a fairly clear consensus emerged from our respondents. For LASIK, 57% answered that a thickness of 300 to 250 μm was right, while 32% chose 350 to 300 μm. Thus a total of 89% identified the thickness range of 350 μm down to 250 μm as desirable. Only 4% chose greater than 350 μm and 7% chose less than 250 μm (Figure 3).
For PRK, too, a clear trend emerged: 48% of respondents identified a thickness of less than 400 μm as desirable, and an additional 30% chose 450 to 400 μm. Fourteen percent chose 475 to 450 μm; the remaining 8% chose greater than 475 μm.
Dr. Donnenfeld pointed out, though, that decision as to how much stromal bed to leave depends on a few factors, age and topography being chief among them. As he put it, a 45-year-old with normal topography will almost certainly not develop keratoconus and so can tolerate a thinner stromal bed, whereas a 20-year-old with an identical topography and refraction very well might develop keratoconus, and so it behooves the surgeon to leave a thicker stromal bed.
Flat vs. Steep
How flat/steep you can make your Ks with corneal refractive surgery is always a complex issue. Surgeons are concerned about what happens to quality of vision if the cornea is made “too” flat — but at what point does that occur? On the question of “How low will you go?” the majority of respondents seemed to agree that they would not go under 35 — fully 48% gave this response (Figure 5). The next most common choice, with 28% of the vote, was a range of 30 to 35, while 15% said that it did not matter.
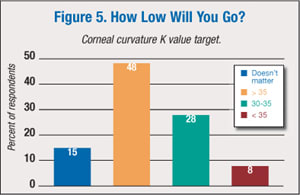
Again, access to latest-generation refractive technology probably affected surgeons' responses. Dr. Donnenfeld said that the advances in design of the ablation profiles give him confidence to make the cornea flatter than he would have with a standard laser. Whereas “in the old days,” he would not go flatter than 35, he will now go to 33.5.
In procedures that steepen the cornea, 56% of respondents chose a preferred range of 48-50 K. Twenty-four percent were willing to go below 48 K and 12% chose a K reading greater than 50. Eight percent responded that the degree of steepening did not matter.
Dr. Trattler voiced a concern that going over 50, or even 48, seemed to result in thinning of the central epithelium that lead to something like the “nipple effect” of superficial punctate keratitis and poor visual quality.
Pupil Concerns
The impact of pupil size on refractive surgery may be one of those cases in which old perceptions die hard. As Dr. Trattler put it, back when conventional LASIK was the refractive procedure, patients with large pupils and high myopia did have more starbursts on testing; however, with the ascent of wavefront-guided treatments, that concern is largely no longer an issue.
Perhaps because some refractive surgeons are still performing conventional LASIK, or maybe as a hangover from the pre-wavefront days when some surgeons were sued based on pupil size and outcomes, 53% of our audience answered that they did indeed worry about refractive surgery on patients with large pupils. Thirty-three percent of audience members at the lecture said that they do not worry about these patients, and 14% answered that they sometimes will not perform the surgery.
PRK Preferences
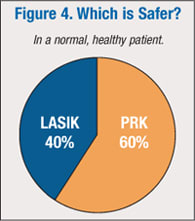
Though LASIK may get the lion's share of press, many in our audience indicated that PRK is their procedure of choice in certain instances.
Sixty percent said that in a normal patient, PRK was safer than LASIK. Forty percent chose LASIK. (We didn't offer an answer of “about the same.”) For moderate-to-severe dry eye patients who have been pretreated with cyclosporine and punctal occlusion, 61% of respondents chose PRK and 25% chose LASIK. Fourteen percent chose, “I would not operate on this patient”
Dr. Slade was not surprised at the responses, pointing out that LASIK contributes to neurotrophia of the cornea in a way that PRK does not.
Similarly, when asked which method they would use to enhance patients who had previously had RK, PRK or LASIK 10 years ago, PRK was the hands-down winner, with 79% of the vote. LASIK was far behind at 16%, while 5% chose “other.”
On the other hand, when asked what was their refractive procedure of choice, 89% of respondents cited LASIK. PRK was a distant second with 11%; LASEK and EpiLASEK each received 0%. And when it comes to enhancing patients after insertion of a premium IOL, it was a draw: 49% of respondents chose PRK, while 51% chose LASIK.
Postop Infection Rates
Sixty-three percent of respondents reported having had a postop infection, roughly equally distributed between PRK and LASIK — 26% vs. 32%, respectively. Forty-two percent indicated they had had infections in more than one type of procedure. However, our sample size for this question was only 40. Further, as Dr. Doane pointed out, given that PRK involves an exposed stroma with the first line of defense against infection not intact until post-op day five, it seems logical that PRK would have a higher infection rate than LASIK, where the gutter is healed at 12 hours.
One more factoid that surprised me: when we asked the audience if they wore gloves, 74% said yes… and 26% said no. As someone who has studied microbiology, endophthalmitis and corneal ulcers, that one puzzled me, but there it is. Fifty-two percent of those surveyed scrub between every case, 14% scrub if they leave and then reenter the surgical suite, and 34% do not scrub.
| A complete audio recording of the 2009 “Controversies in Refractive Surgery” course can be purchased at the Association of Cataract and Refractive Surgeons Web site: http://store.avmg.com/products.cfm?conf_id=505&client_id=28. |
Keratome Trends
Turning to keratome preferences, the femtosecond (FS) lasers continue to gain ground, with 40% of respondents saying that they used only the FS laser. Only slightly more, 42%, said they only used a microkeratome. Twelve percent said that they use both in selected patients, and the remaining 6% said that they only perform PRK. So the number of FS laser users is slightly higher than it was last year, when I believe it was 33%.
Mitomycin C: Who and When?
On the subject of prophylactic mitomycin C (MMC), responses were all over the board, particularly on duration of exposure. We still don't have a conclusive study on how much to use for how long. But despite that, only 5% of respondents said they did not use MMC (Figure 6).
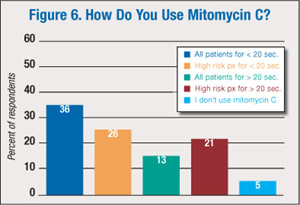
Dr. Slade said he uses it on any patient with prior history of corneal surgery. And while most respondents said they use MMC for less than 20 seconds, Dr. Trattler said he bases his time of exposure on the cornea on the patient's occupation — patients whose livelihoods require significant UV exposure may get up to 45 seconds of MMC.
Use of MMC seems to be catching on among refractive surgeons; in last year's course, the number of respondents who indicated they didn't use it was 7%, two points higher than this year. As we discussed above, a lot of surgeons are using PRK for an enhancement tool — but before mitomycin C, we would never have done that.
ICLs Still Not Embraced
When asked if they use ICLs, 64% of our audience said no. Only 36% said yes. I suspect this is because surgeons are simply not comfortable with the ICL choices we currently have. I think they continue to be concerned about endothelial cell loss and cataract formation. An additional factor is probably that many true refractive surgeons do not perform intraocular surgery and only offer corneal options.
Presbyopia Preferences
On the topic of corneal presbyopic solutions, you hear of people doing a lot of different things: working on the surface of the cornea — whether that means implanting an intracorneal option or CK — or refractive lensectomy which more and more patients seem to be choosing.
When we asked our audience what they thought the best solution to presbyopia is, refractive lens procedure won in a landslide — 73%. The next closest choice was a corneal refractive procedure, at 22%, with intracorneal refractive procedure getting 5% of the vote and CK getting 0%.
Two surgeons I know who have actually shown an increase in their LASIK volume over the last quarter are doing what's called “progressive multifocal LASIK.” Basically what they're doing is increasing negative asphericity. The surgeons are getting good results. The patient's postoperative visual acuity at distance is hovering between 20/20 and 20/25, and they are reading around J2 to J3 in the majority of the cases. So I think that's something we are going to see more and more of in the years to come.
Join Us Next Year
At next year's course, we plan to add more videos and more “catastrophes” for the audience to analyze and compare notes on. I hope to see you there! OM

|
Karl G. Stonecipher, MD practices at Southeastern Eye Center in Greensboro, NC, and lectures regularly on refractive surgery techniques. He can be reached via e-mail at: stonenc@aol.com. |








