Pearls for Patient Happiness
Implement these strategies for delivering a premium experience in the new era of cataract surgery.

BY UDAY DEVGAN, MD, FACS
The sun has set on the old days of cataract and implant surgery. In the past, our typical patient was elderly, had a dense cataract, very poor vision and an "I want Medicare to pay for it" attitude. Given that mindset and the IOL technologies that were available, patients had a narrow range of sharp uncorrected vision postoperatively.
Today, we see younger patients who are working, driving and leading active lives. They're likely to have milder cataracts and relatively good visual acuity, but they're looking for more. They may be self-paying and seeking refractive lens exchange. With this new mindset and premium IOL technologies, we can provide patients with a wider range of sharp uncorrected vision.
In my practice, the key to success in this new era of cataract surgery lies in something Richard Lindstrom, MD, has said about LASIK: "Don't obsess over 20/20; just get 20/happy." Here, I explain how to make premium IOL patients "20/happy." I employ several strategies, which fall into three main categories: educating and guiding patients, providing a great experience and increasing refractive accuracy.
Educate and Guide Patients
To educate patients and guide them toward the procedure that's best for them, I take the following steps:
■ Maintain an educational Web site. At my practice's Web site, www.maloneyvision.com, patients can access information about eye anatomy and cataract surgery in general. They can watch videos of my partner and me discussing how cataract surgery has changed over the years. They can see videos of other patients, including celebrities I've treated, talking about their experiences with the practice. They can read about IOLs, including multifocal and accommodating options. We let every patient know about this easy-to-use, 24-hour resource.
■ Mail informative literature. Before coming to the office to discuss the procedure, each of our cataract surgery patients receives information in the mail about cataract surgery and refractive lens exchange. Informed patients are more knowledgeable partners in their care, and they're often more comfortable with the surgical procedure and the end results.
■ Understand what your patient wants to achieve. It's crucial to use a questionnaire or survey, such as the one developed by Steven J. Dell, MD, to determine what each patient wants. For example, is near, distance or intermediate vision the priority? For what activities would he like to be spectacle-free? Is there a situation in which he doesn't mind wearing corrective lenses? It's helpful to have the patient rate his personality on a scale from easy-going to perfectionist. Perfectionists are more difficult, sometimes even impossible, to please. The questionnaire, along with talking to the patient, helps me determine if expectations for postoperative vision are unrealistic and therefore not in anyone's best interests to pursue.
■ Set realistic expectations. Here, I take a cue from my two sisters who are plastic surgeons. They tell the 65-year-old Mrs. Jones they can make her look better, but not like she did when she was 21. Along the same lines, I don't promise patients the visual function of a teenager. I explain that I can make them see better, but not as well as when they were 21. I don't have the Fountain of Youth at my disposal.
More specifically, I say that after surgery, 95% of patients will see well without eyeglasses for 95% of daily activities. I discuss what visual functioning is reasonable to expect and what is not (Figures 1 and 2). It's reasonable to expect to be able to read the newspaper in good lighting, drive and see your cell phone and computer screen without eyeglasses. It's not reasonable to expect to be able to read the back of the sweetner packet by candlelight without eyeglasses. Also, I've found it useful to make sure patients understand that after surgery, it's still perfectly OK to wear reading eyeglasses when they need them. Some seem to need that permission.
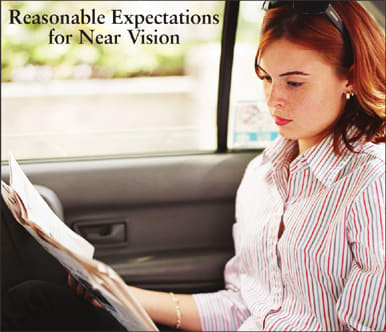
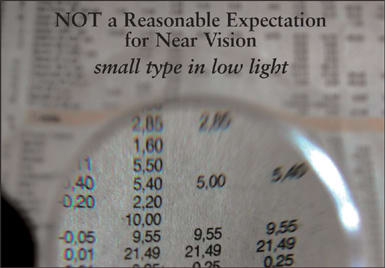
Figures 1 and 2. Surgeons must educate patients, so their expectations regarding postoperative vision will be realistic.
■ Make the IOL recommendation. When I take my car to the shop for brakes, I don't know whether to get slotted rotors, dustless pads or upgraded calipers. I want the mechanic to tell me what's best for my car, because he's the expert in the field. I keep this in mind with my cataract surgery patients. I avoid giving them a long list of options and forcing them to choose one. Based on eye anatomy, measurements, vision goals and so on, I tell them which lens is best for them.
Provide a Great Experience
Patients decide how satisfied they are with our services based on a number of factors. Therefore, we try to ensure their experience with the practice and their procedure is pleasant by doing the following:
■ Treating patients like family. To put it simply: Be nice. Johnny Gayton, MD, says, "Patients don't care about how much you know, until they know how much you care."
■ Addressing postop issues. Any questions or concerns patients raise should be taken seriously. If a patient has a concern, it needs to be addressed and resolved. In some cases, a great deal of hand-holding is necessary.
■ Spending enough chair time. I spend about 1 hour with patients on their initial visit, giving them a detailed education, examination and explanation. The patient, the surgeon and the staff need to be on the same page before surgery.
■ Being accessible. Patients want access to the doctor. I give all patients my real e-mail address and my actual cell phone number. Patients will respect your privacy and will only call when there are urgent issues, but the gesture goes a long way toward doctor-patient trust.
■ Adopting new technologies conservatively. When I'm starting out with a new IOL or a new technique, I begin with the least demanding patients for whom the results will be most predictable. This usually means hyperopes with cataracts and low astigmatism who also happen to be easygoing.
■ Eliminate discomfort and other issues that compromise postop vision. I use nonsteroidal anti-inflammatory drops not only to combat cystoid macular edema but also to relieve itching and burning. I check the ocular surface for conditions such as dry eye and blepharitis and treat before surgery when necessary. I stay alert to dry eye postop, too, because cutting corneal nerves during surgery can induce a relative dry eye state. Light is focused by the tear film first, so the tear film must be healthy. And remember, it's rarely necessary to inconvenience patients by having them wear an eye patch after their procedure.
■ Decrease the intraoperative complication rate. It makes no sense to promise premium results from a premium procedure and IOL and then allow intraoperative complications to occur. For example, to reduce my chances of breaking the capsule, I've switched from the traditional steel to the soft siliconecoated irrigation/aspiration tips.
Increase Refractive Accuracy
Refractive accuracy is key to premium IOL performance. There are no shortcuts. Close attention to detail is required in all of the following areas.
■ IOL calculations. Now that cataract surgery is refractive surgery, it's more important than ever to perfect lens calculations. Use optical coherence biometry or immersion ultrasound for accurate A-scans, and personalize the A constant. I use a different formula depending on the case.1,2 For example, I choose the Hoffer Q for axial lengths shorter than 22 mm, an average of three formulae for 22 mm to 24.50 mm, Holladay I for 24.51 to 26 mm, and SRKT for axial lengths longer than 26 mm (Figure 3). The Holladay 2 formula is a 7-variable formula that also provides a high degree of accuracy.
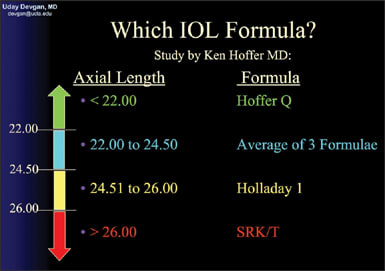
Figure 3. For precise IOL calculations, I choose a formula based on axial length.
■ Nomograms. We develop our own nomogram for our LASIK patients, so why not for our IOL patients? The nomogram should be personalized to the patient, the technique and the IOL.
■ Post-LASIK eyes. True K power must be determined as accurately as possible. There are many methods for determining it, but none of them are perfect. In the absence of a clinical history, I've found the most accurate formula to be one described by Douglas D. Koch, MD,3 which requires the central K reading from topography or the average of the 0-3 mm zones. Web sites to help guide IOL power adjustment, such as iol.ascrs.org and iol.ocularmd.com, may be useful. In post-LASIK eyes, I prefer to err on the side of myopia.
■ Postop surprises. Cataract patients with a refractive mindset want to be emmetropic or plano, so they may not accept even a slight postop refractive error. Therefore, you must be able to fine-tune results. Options include IOL exchange, a piggyback lens, PRK, LASIK or conductive keratoplasty. I prefer using LASIK or PRK. If you're not comfortable performing these procedures, collaborate with a local refractive surgeon. In my practice, up to 10% of patients need an enhancement to be completely satisfied.
■ Astigmatism. The difference between unhappy and happy patients with the same spherical equivalent is often cylinder or no cylinder. Know the astigmatic effect of your incisions. Look at the charts of your last 20 patients and compare the pre- and postop K values. Most surgeons induce a flattening of about half a diopter on the axis of the incision. You may be able to address mild cases of astigmatism by simply making your incision on the steep axis. For larger degrees of cylinder, it's helpful to use limbal relaxing incisions or a toric IOL.
Under-promise and Over-deliver
To provide what today's cataract surgery patients want, it's necessary to under-promise and over-deliver. Using the strategies I've outlined here, you should be able to do just that. ■
Dr. Devgan is a partner in Maloney Vision Institute in Los Angeles, chief of ophthalmology at Olive View UCLA Medical Center and associate clinical professor at UCLA School of Medicine's Jules Stein Eye Institute. You can reach him at devgan@ucla.edu.
References
- Hoffer KJ. Clinical results using the Holladay 2 intraocular lens power formula. J Cataract Refract Surg. 2000;26:1233-1237.
- Hoffer KJ. The Hoffer Q formula: a comparison of theoretic and regression formulas. J Cataract Refract Surg. 1993;19:700-712.
- Koch DD. New options for IOL calculations after refractive surgery. J Cataract Refract Surg. 2006;32:371-372.








