Using the 3-D Wave™ in Cornea And IOL Applications
This surgeon used the 3-D Wave to more accurately diagnose and treat patients.

By Thomas John, MD
User-friendly, automated ophthalmic testing equipment that saves time and requires little space is always welcome in any ophthalmology practice. The 3-D Wave (Marco), certainly fits these criteria. I find this unit to be a useful clinical tool in evaluating the anterior segment and the entire optical system. The 3-D Wave is extremely accurate and can be coupled with the EPIC 5100 or TRS 5100 refracting systems. It provides a one-stop-shop approach to a comprehensive eye exam that most ophthalmologists will appreciate. It's an autorefractor, keratometer, corneal topographer, pupillometer and wavefront aberrometer all in one unit. These fast, complex composite measurements often can help you perform an objective evaluation of a patient's symptoms and come to a more definitive clinical diagnosis. This enables you to assess patient complaints, manage various ocular conditions and improve best-corrected visual acuity. It's an essential diagnostic tool in the office setting.
In this article, I'll share some clinical examples of cases that underscore the utility of the 3-D Wave device.
Case 1: Good Vision But Persistent Symptoms
A 47-year-old Caucasian man was referred to me by a retina specialist for evaluation of his cornea and anterior segment for unexplained ocular symptoms. The patient complained of blurred vision in his left eye for about 5 months. He had a history of repaired bilateral retinal detachments. In his left eye, he had retinal detachment surgery with the use of silicone oil in March 2008. The silicone oil was removed from his left eye about 2 months after surgery. He complained he couldn't see with his left eye in bright light but could see better with his pupil dilated in dim light.
The patient's uncorrected vision in the symptomatic left eye was 20/30-2. The uncorrected vision in the asymptomatic right eye was 20/60-2, which improved to 20/40-2, using the pinhole. The clinical exam in the left eye revealed a clear cornea, a well-centered posterior chamber IOL and an attached retina. He also had a history of blurred vision in his left eye. Normally, one would question the symptoms in the patient's left eye, because of the excellent surgical result and the uncorrected visual acuity of 20/30-2. I tested both of the patient's eyes with the 3-D Wave and examined his cornea and retina in his left eye using optical coherence tomography (OCT).
Uncovering the Problem
The 3-D Wave wavefront analysis showed abnormal total aberrations and point spread function (PSF) in the left eye compared with the right eye (Figures 1 and 2). OCT showed macular thickening in the asymptomatic right eye and a normal macula in the symptomatic left eye. OCT showed normal corneas in both eyes. The total aberrations in the right eye were 1.628 and 8.366 in the left eye. Based on the 3-D Wave wavefront analysis, I reexamined the patient clinically after pupillary dilation. A red reflex exam showed a silicone oil droplet on the posterior IOL surface. This oil droplet contributed to his ocular symptoms. I sent the patient back to his retinal surgeon to correct the problem.

Figure 1. Wavefront analysis of the right eye, using the 3-D Wave, shows a total aberration of 1.628. The point spread function also is shown. |

Figure 2. Wavefront analysis of the left eye shows a total aberration of 8.366 and a grossly abnormal point spread function. |
This case demonstrates that without the use of wavefront analysis using the 3-D Wave, I wouldn't have uncovered the true etiology of his ocular symptoms, and the patient might have gone from doctor to doctor without ever receiving the proper diagnosis and treatment. His symptoms would've been discounted because his uncorrected visual acuity was excellent after retinal detachment surgery with silicone oil.
Case 2: Confirmation of Corneal Ectasia
A 45-year-old man underwent LASIK in both eyes. He presented with a history of blurred vision in his right eye. His uncorrected vision in the symptomatic right eye was count fingers. He had numerous metallic, nonreactive, small foreign bodies in the corneal interface between the flap and the bed. The 3-D Wave corneal topography exam confirmed corneal ectasia in the right eye. The PSF was abnormal, and the total aberrations in the right eye and left eye were 6.512 and 2.378, respectively. He underwent total anterior lamellar keratoplasty in his right eye (Figure 3), retaining his healthy corneal endothelium, thus preventing any future endothelial graft rejection and surgical correction of the corneal ectasia.
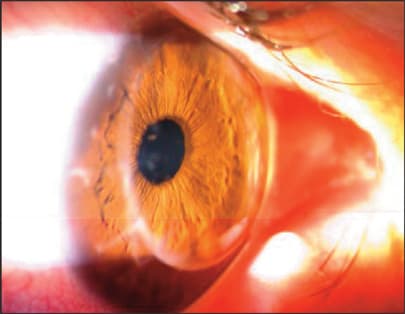
Figure 3. This image shows a clear cornea with no ectasia after total anterior lamellar keratoplasty for the correction of corneal ectasia after LASIK.
The 3-D Wave topography confirmed the diagnosis of corneal ectasia in the patient's right eye and showed poor quality of vision with abnormal PSF and increased total aberrations.
Case 3: Preventing Surgical Intervention
A 55-year-old Caucasian woman underwent Descemet's stripping automated endothelial keratoplasty with phacoemulsification and posterior chamber IOL implantation in both eyes under topical anesthesia with monitored anesthesia care. Her uncorrected visual acuity was 20/100 in the right eye, which improved to 20/40 using the pinhole. Her uncorrected visual acuity was 20/30 in her left eye. The patient complained of blurred vision in her right eye. Biomicroscopic examination revealed macro- and micro-folds in the donor disc that was clear and well adherent to the patient's cornea (Figure 4). I considered a corneal disc exchange in her right eye. The 3-D Wave analysis of the cornea showed increased total aberrations in her right eye. The total aberration 8 months after surgery was 2.226 with a dK of 0.66, and the total aberration at 1 year and 6 months after surgery was 1.704. The patient's symptoms improved over time.
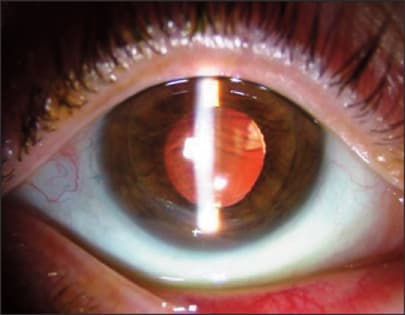
Figure 4. This image shows macro- and micro-folds in the clear, donor corneal disc following Descemet's stripping automated endothelial keratoplasty.
The 3-D Wave topography confirmed the remodeling of the donor-recipient corneal interface with decreased total corneal aberrations over time, thus improving her ocular symptoms. This test helped me decide to observe the patient instead of performing a corneal disc exchange.
Useful, Investigative Tool
The 3-D Wave certainly is a useful, clinical investigative device that can assess corneal topography, evaluate the optical system and calculate higher- and lower-order aberrations and more. Such an instrument helps in the clinical diagnosis of various corneal and anterior segment diseases. In addition, physicians can use the 3-D Wave sequentially over time to evaluate response to treatment, progression of keratoconus and iatrogenic corneal astigmatism after penetrating keratoplasty. Clinicians also can use this unit in presurgical applications to screen for keratoconus or pellucid marginal degeneration, which are contraindications to LASIK. You can use the 3-D Wave for pupillary evaluations and documentation and to evaluate the quality of vision in patients after cataract surgery. The 3-D Wave is a multifunctional unit that's an essential clinical tool in any eyecare practice. OM
Dr. John is clinical associate professor at Loyola University in Chicago, and he's in private practice in Tinley Park and Oak Lawn, Ill.
The OPD-Scan II (3-D Wave) is manufactured by Nidek.








