Spotlight on Technology & Technique
MG Probing: Immediate Results for a Chronic Problem
By Leslie Goldberg, Associate Editor
Ophthalmologists have long been frustrated by a lack of understanding of meibomian gland dysfunction (MGD) and the less-than-satisfactory therapeutic options available to their patients.
Tampa's Steven L. Maskin, M.D., who has focused on dry eye and ocular surface diseases since 1991, says that after years of facing patients with limited options to relieve their complaints due to chronic obstruction of these glands, he decided he would try to innovate a way to physically get inside the individual gland and remove blockages. Symptomatic improvement should result.
"I hypothesized that I could relieve patients' symptoms by finding a way to enter the gland and relieve the obstruction without altering the tissues," says Dr. Maskin. "I did not want a destructive process and did not want to use sharp instruments or adjunctive energy that would alter my findings."
Breakthrough
Dr. Maskin developed instrument prototypes to test his theory and used these investigational designs (with proper informed consent) on some of his MGD patients. His findings were a breakthrough in the understanding and management of MGD, he says.
First, he found that he could easily enter the MG and, with the probing technique, immediately and dramatically relieve symptoms. Secondly, he found through probing that the conventional understanding of MGD was "incomplete at best."
"The focus on treatment in the past was to remove obstructed meibum with heat and massage and to improve the quality of the meibum using antibiotics, anti-inflammatory agents and omega-3 fatty acids. Moreover, gland obstruction was thought to be related to keratinization of the ductal epithelium and orifice," says Dr. Maskin. "But when I entered the gland and began probing, there was resistance deep inside the main duct — similar to that of a scar that I could penetrate through, with release of sequestered meibum."
He concluded that in MG disease, obstruction could develop deep within the gland, not only or simply due to cells that had keratinized, but as a result of growth of fibrotic and neovascular scars and membranes within the duct, which is a new concept.
Dr. Maskin explains that any chronic inflammation can lead to growth of new blood vessels and scarring (as seen in macular degeneration). "Since we had never entered the MG in vivo, this was not contemplated. Once I could enter the gland, find the resistance to the probing, and penetrate through and relieve that blockage — it suggested there was a fibrotic or neovascular scar or membrane traversing the duct." His patients' congestion inside the lids, which led to their tenderness, was immediately relieved by probing.
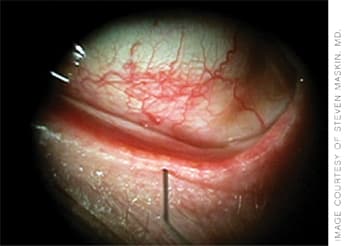
A 2-mm probe almost fully inside the meibomian gland, re-establishing patency of the duct.
Once Dr. Maskin's findings and successful results were repeatable and reliable, he identified Rhein Medical as a partner that could commercially develop his probe and market it for routine in-office use.
The MGD Treatment Process
First, Dr. Maskin says, it is extremely important that the doctor put his finger or a cotton swab on the lid at the slit lamp to elicit lid tenderness, a sensitive marker of inflammatory MGD. He recommends pressing the nasal, central and temporal glands through the lid. He starts gradually and may only probe the most sensitive section.
Dr. Maskin begins with the least invasive probe (which is 2 mm). He finds that the amount of discomfort varies from patient to patient depending on the severity and chronicity of the disease but that once the process is started, patients generally allow him to proceed because the improvement is immediate. If there are signs of lid inflammation such as congestion or tenderness, he says to first probe to establish duct patency, then preserve the functioning patent ductal system with adjunctive oral antibiotics and omega-3 fatty acids plus anti-inflammatory agents and warm compresses. "We need to arrest the inflammatory reactions and restore tissues to a healthy state," says Dr. Maskin.
"Now that our technology has enabled us to move inside the meibomian gland duct, I am evaluating intraductal pharmaceutical injection using tubes that can be inserted through the orifice, also available from Rhein Medical," says Dr. Maskin. "Furthermore, this technology should unlock new areas of research to advance our knowledge of the healthy and diseased meibomian gland," he suggests.
Early Results
Dr. Maskin is currently following an initial group of 25 patients with MGD that received therapeutic probing. He has found that once the original procedure had been performed, 20 patients did not require re-treatment by their 11-month follow-up. The five requiring re-treatment were again probed at 4.6 months on average.
Dr. Maskin's ARVO poster states that lid tenderness was noted in 80% of subjects. Five of the 25 patients did not have lid tenderness but had symptoms suggesting lid margin congestion. Dr. Maskin's patients complained of heavy lids, irritation, gummy lids and lid awareness. Once examined, he saw the congestion of the lid and probed with success.
"When patients came back for follow-up, many said — unsolicited — that they had less friction on the eye when they blinked, had less need for artificial tears and less light sensitivity," says Dr. Maskin. "Patients may develop subclinical symptoms of MGD and not realize it because of its gradual onset. Only when relieved, do they realize what had developed. This disease is chronic with gradual onset, but if obstruction and inflammation continue, it can lead to gland atrophy and loss of architecture."
Dr. Maskin says that even if the lid margin is scarred and glands are partially atrophic, if he can find an orifice and duct to probe, he can create significant symptomatic relief. OM
For more information on the device, contact Rhein Medical at (813) 885-5050. Dr. Maskin may be contacted at (813) 875-0000.








