Making Optimal Use of the 3-D Wave™ in Refractive and Cataract Surgery Applications
Here's how this ophthalmologist maximized visual outcomes in a variety of patients.

By James J. Salz, MD
I've had the Marco 3-D Wave for about 2 years, and it's probably the most frequently used instrument in my busy practice at the American Eye Institute in Los Angeles. The Marco 3-D Wave is a combined autorefractor, keratometer, corneal topographer, wavefront aberrometer and light and dark pupillometer, making it a multifunctional diagnostic instrument.
We perform autorefractions with the Marco 3-D Wave on all new patients who require a complete eye exam. The autorefraction takes just a couple of minutes and provides our technicians with an excellent starting point for performing refractions. The instrument has helped decrease the time it takes for the technicians to provide a complete workup, because it enables them to start with a refraction that's very close to the patient's final prescription.
In addition, the 3-D Wave helps us better evaluate potential refractive and cataract surgery patients, as well as manage astigmatism, and it enables us to generate more income. This article will explain how I use the Marco 3-D Wave and how it benefits my patients and my practice.
Evaluating Refractive Surgery Candidates
We use the 3-D Wave for all patients who come in for refractive surgery consultations. We perform refractions and obtain keratometry, corneal topography and wavefront aberrometry readings. Previously, we had to use three separate instruments in different exam rooms to obtain this information, which took about 10 minutes. Since the 3-D Wave combines the capabilities of five instruments, we can complete diagnostic tests in about 2 minutes in just one exam room. The graphic information the 3-D Wave provides makes it easy for us to explain to patients whether or not they're good candidates for refractive surgery, and if they're best suited for custom wavefront-based LASIK or conventional LASIK.
Cataract Patient Workup
When evaluating cataract patients before surgery, we perform autorefractions and obtain keratometry, pupillometry, topography and wavefront readings. We also calculate and print out corneal spherical aberration and total spherical aberration measurements. We explain to patients that these findings enable us to give them the best possible visual outcome.
In addition, I review the results of the 3-D Wave tests with patients and the findings from the IOL Master. I explain the IOL Master readings are essential in calculating lens power. I discuss the topography results. And if they have little or no astigmatism, I explain that I can make an incision in the normal temporal location, and that additional incisions or a toric lens implant won't be necessary. If they have astigmatism, I demonstrate that I can correct the astigmatism with eyeglasses after surgery or attempt to reduce the astigmatism with LRIs or a toric lens implant. For years, I didn't charge patients for topography and LRIs, but in order to generate additional revenue for my practice, I began charging patients for both procedures.
Lastly, I show patients the results of their wavefront test and explain that the readings for spherical aberration help me choose a spherical or aspheric lens implant.
| Case 1 |
|---|
The refraction of this cataract patient was -3.50 -1.00 × 15 OD with a best-corrected visual acuity of 20/60. The topography of this patient showed asymmetrical astigmatism of 2.59D with more steepening superiorly. The superior limbal relaxing incision at 115° was 2 o'clock hours in length. The inferior incision in the same axis was 1 o'clock hour in length at a blade setting of 600 microns. Postoperative uncorrected visual acuity was 20/25 in this dominant right eye targeted for distance. The target for his post-op refraction OS was -1.50D. Topography showed a similar asymmetrical astigmatism of 2.34D. Again, I performed asymmetrical LRIs. His refraction was -1.00D post-op in his nondominant left eye targeted for monovision.
The topography of this patient shows 2.34D of asymmetrical corneal astigmatism OD, which were corrected with limbal relaxing incisions. |
| Case 2 | ||
|---|---|---|
| The refraction of another patient who required cataract surgery was +1.75 -5.00 × 18 OS. His best-corrected visual acuity was 20/80. The topography of this patient showed symmetrical astigmatism of 3.58D. I performed symmetrical LRIs that were 3 o'clock hours in length above and below the cornea at 95°. Postoperatively, his refraction was -1.00 -0.50 × 180. | ||

|
The topography of this patient shows 3.58D of symmetrical corneal astigmatism (left). Symmetrical LRIs 3 o'clock hours in length above and below (right) improved the refraction. |

|
| Case 3 |
|---|
I performed PRK 8 years ago on the following patient who had -9.00D of myopia. She later developed a cataract in her left eye that caused her refraction to become more myopic at -5.00D. Her best-corrected visual acuity was 20/50. The map below shows the typical central flattening of a patient with myopic PRK. And as expected, she had positive corneal spherical aberration of 0.203. I implanted an aspheric lens (Alcon AcrySof IQ SN60WF) targeted for monovision at -1.50D in the nondominant left eye. Her postoperative refraction is now -2.00D.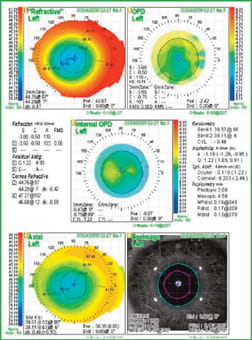
This topography map shows typical central flattening of a patient who had myopic PRK. Her positive spherical aberration of 0.203 was corrected with an aspheric lens (Alcon AcrySof IQ SN60WF). |
| Case 4 |
|---|
I performed LASIK in another patient 8 years ago for hyperopia. She developed a cataract in her right eye. Her bestcorrected vision was 20/70 with a plano refraction. Her topography shows the typical central steepening of hyperopic LASIK, and as expected, she has negative corneal spherical aberration of -0.131. The implant I chose was a spherical lens (Alcon AcrySof SA60AT) in this nondominant eye with a target of -1.50D. Her final refraction is -1.25D.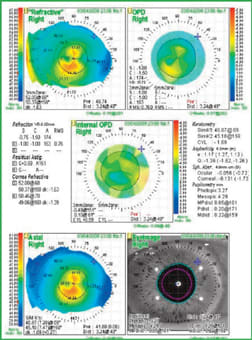
This topography map shows typical central steepening of hyperopic LASIK. The patient's negative corneal spherical aberration of -0.131 called for a spherical lens (Alcon AcrySof SA60AT) correction. |
Valuable and Profitable Instrument
The Marco 3-D Wave has been a valuable addition to my practice. The technicians find the instrument easy to use with minimal training. It helps us to quickly evaluate our refractive surgery patients and produce additional income for cataract patient workups. For example, if we only used the Marco 3-D Wave to evaluate 10 cataract patients a month, we'd generate $900 (covering the average lease payment). If three patients choose to have LRIs, we can collect an additional $750 for a total of $1,650. Currently, my practice performs these evaluations on 350 cataract patients each year. Aside from the extra revenue, the instrument helps us produce better visual outcomes for cataract patients, manage astigmatism and select the appropriate lens implant based on topography, spherical aberration of the cornea and wavefront aberrometry readings. OM
Dr. Salz is clinical professor of ophthalmology at the University of Southern California. He's president of Laser Vision Medical Group in Los Angeles, and partner with the American Eye Institute in Los Angeles. He's been principal investigator in nine FDA laser vision correction studies and has published articles and lectured extensively on all aspects of refractive surgery.








