Seeing Both Sides of Glaucoma
New diagnostic technology can corroborate subjective findings, but what should you do when there's a mismatch? Two experts explain.
BY STEVEN MANSBERGER, MD AND CHRISTOPHER BOWD, PhD
Some ophthalmologists may remember the days when we only needed to interpret intraocular pressure and perimetry in deciding whether our patients with glaucoma were stable. Today, eyecare providers must interpret myriad clinical and diagnostic data when evaluating our glaucoma patients, and particularly when making treatment decisions.
In recent years, diagnostic testing has become increasingly important when evaluating the glaucoma patient. Standard automated perimetry (SAP) has been augmented by the more sophisticated algorithms of short-wavelength automated perimetry (SWAP) and frequency-doubling perimetry (FDT), as well as electrophysiology. In addition, fundus examination has been augmented by structural testing with the Heidelberg Retinal Tomograph (HRT), ocular coherence tomography (OCT), and retinal nerve fiber layer birefringence assessment (GDx). These techniques can provide clinicians with an entirely new perspective on glaucoma detection and progression.
How do eyecare providers interpret discordant results between functional and structural testing? In this article, we hope to give you guidance about how to manage your glaucoma patient when functional and structural testing do not agree.

|

|
The images in this article present a multitude of diagnostic information — much of it conflicting — from a glaucoma patient with a small optic disc (1.2 mm2 by HRT). The left photo shows no indication of structural damage while a dramatic superior field defect is evident by SAP (right).


Two views of the HRT Moorfields Regression Analysis results are shown above. Borderline rim thinning in the inferior and inferior temporal regions correspond with the superior visual field defect.
ALL IMAGES COURTESY OF CHRISTOPHER BOWD, PH. D.Mixed Signals
Discordance between structural and functional testing is possible both at initial diagnosis as well as in tracking disease progression in known glaucoma patients.
• What do you do if your structural test shows an abnormal result, but the visual field is normal?
First, you should check that your operator has performed the testing accurately. For example, the HRT can give an abnormal Moorfields result from a misplaced contour line, and the OCT retinal nerve fiber thickness may be abnormal if the operator does not center the testing on the optic disc. All of the machines will show an abnormal result in optic discs that have unusual appearances such as anomalous, tilted, or macrodiscs.
If your operator has performed the structural testing accurately, one should consider a diagnosis of pre-perimetric glaucoma, i.e., glaucomatous structural abnormalities without an abnormal visual field. To investigate pre-perimetric glaucoma, we recommend a selective functional test with SWAP or FDT. Both of these tests isolate a subset of ganglion cells, and studies show that they can be predictive of future functional loss.1 If these tests remain normal, one can consider monitoring the patient without treatment. This exhaustive testing should be reassuring to the doctor and patient. In the future, these baseline results will be important for detecting change to the structure and/or function at an early stage of glaucoma. To date, studies have not documented the early detection ability of electrophysiology testing for glaucoma.
• What do you do if a structural test shows change over time, but the visual field remains normal?
Consider the recommendations listed above, and also repeat the objective structural tests. All of these tests have variability, which can give a false positive result for glaucomatous structural change. If the change in structure is confirmed, eyecare providers should consider advancing therapy and lowering the IOP further.
Another important concept to consider is whether optic disc hemorrhages represent a change in structure. Optic disc hemorrhages may occur without a change in function. The Ocular Hypertension Treatment Study (OHTS) showed that only 14% of ocular hypertension patients with a hemorrhage had visual field progression over 8 years;2 the Early Manifest Glaucoma Treatment Trial showed that >50% of glaucoma patients had a disc hemorrhage and more than 80% of them (as compared to 67% without) progressed over an 8-year period;3 finally, a retrospective study showed a 90% probability of progression over a similar period when a disc hemorrhage occurred.4
|

|
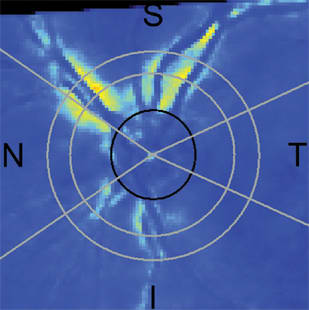
GDx retardation image (left) with deviation from normal plot (right), show obvious inferior RNFL thinning.
Overall, ophthalmologists should recognize that optic disc hemorrhages are an important risk factor for glaucomatous progression. If IOP is controlled, attempt to determine whether the patient is being compliant with their medications because a hemorrhage may represent poor IOP control during the preceding months. We recommend photographing the hemorrhage and monitoring for structural or functional progression. If the patient has an optic disc hemorrhage and the IOP is uncontrolled, advance therapy with additional medications, laser, or surgery.
• What do you do if the structure appears normal, but you have an abnormal visual field?
The opposite situation is possible as well: a patient can either present with or develop a visual field defect on standard automated perimetry but the optic disc and RNFL can appear unexpectedly healthy on examination.


Additional information on RNFL thinning is evident by Cirrus spectral-domain OCT RNFL thickness plot (left) and deviation from normal plot (right).
What to do? First of all, this is not particularly unusual. In the OHTS, 35% of ocular hypertensive eyes converted to glaucoma based on visual field results alone.5 When a visual field is abnormal and the optic disc and retinal nerve fiber layer appear normal by examination, the first step is to repeat the visual field test. The OHTS showed that 86% of visual field defects reverted to normal on repeat testing.6 Therefore, one should confirm a visual field defect with repeat testing prior to advancing therapy. Not to be overlooked is the importance of the reliability of the tests performed. All visual field printouts must be checked for adherence to reliability standards (usually provided by the manufacturer on the printouts) and the absence of known test-taking artifacts (e.g., rim artifacts).
If the visual field abnormality is deemed reliable and repeatable (i.e., it is "real") and uncertainty over the status of the optic disc remains, the next step is to look more carefully for local abnormalities in disc/RNFL appearance; specifically those that correspond with areas in which the field is abnormal. For instance, an early superior nasal step defect demands increased scrutiny of the inferior temporal rim and corresponding RNFL. This type of logical exam often can detect changes previously missed during a quick global assessment.
Glaucoma experts recently proposed a step-wise approach to evaluate the optic disc and nerve fiber layer. This approach includes five rules based on disc size, neuroretinal rim size and shape, retinal nerve fiber layer, presence of parapapillary atrophy, and presence of retinal or optic disc hemorrhages.7 Using this step-wise approach may help eyecare providers recognize subtle glaucomatous findings.


RTVue spectral-domain OCT RNFL thickness plot (left) with RNFL thickness profile (right), showing further evidence of inferior RNFL thinning.
Even with this added information, detection of subtle disc and RNFL defects can be difficult. In cases such as this, the third step would be to use objective structural testing. The appearance of a normal optic disc varies greatly, so eye care providers may have difficulty detecting abnormalities especially in unusual optic discs. For instance (this is one example of many possible), a small disc in an apparently healthy eye with an average number of nerve fibers will appear crowded (i.e., small to non-existent cup). If this type of eye has glaucoma, considerable rim loss may occur before this loss is apparent by examination.
Recent advances in imaging technologies allow comparison of rim and RNFL measurements to large normative databases, in some cases corrected for optic disc size. The HRT Moorfields Regression Analysis, for instance, classifies eyes as within normal limits, borderline or outside normal limits by rim area accounting for disc area, based on comparison to a normative database. A newer analysis for the HRT, the Glaucoma Probability Score, assesses disc topography without regard for disc area (although both techniques are influenced by disc size, being more sensitive in eyes with larger discs).8
In small, crowded discs where little information may be available about changes in rim thickness, optical imaging-measured abnormalities of the RNFL may prove more informative (in fact, sensitivity is better in eyes with smaller discs using RNFL-specific imaging9). Similar to HRT, GDx scanning laser polarimetry and optical coherence tomography (time- and spectral-domain OCT) for measuring RNFL thickness also provide useful comparisons of measurements to large normative databases. In general, HRT, GDx and OCT normative databases can help put an eye within the context of hundreds of other eyes. Ophthalmologists can use this valuable information to increase (or decrease) confidence in the legitimacy of visual field defects in the presence of an initially healthy appearing optic disc, which can help inform (but should not dictate) treatment decisions. OM
References
- Mansberger SL, Demirel S. Early detection of glaucomatous visual field loss: why, what, where, and how. Ophthalmol Clin North Am 2005;18:365-373, v-vi.
- Budenz DL, Anderson DR, Feuer WJ, et al. Detection and prognostic significance of optic disc hemorrhages during the Ocular Hypertension Treatment Study. Ophthalmology 2006;113:2137-2143.
- Bengtsson B, Leske MC, Yang Z, Heijl A. Disc hemorrhages and treatment in the early manifest glaucoma trial. Ophthalmology 2008;115:2044-2048.
- Rasker MT, van den Enden A, Bakker D, Hoyng PF. Deterioration of visual fields in patients with glaucoma with and without optic disc hemorrhages. Arch Ophthalmol 1997;115:1257-1262.
- Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, Parrish RK, 2nd, Wilson MR, Gordon MO. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701-713.
- Keltner JL, Johnson CA, Levine RA, Fan J, Cello KE, Kass MA, Gordon MO. Normal visual field test results following glaucomatous visual field end points in the Ocular Hypertension Treatment Study. Arch Ophthalmol. 2005;123:1201-6.
- Fingeret M, Medeiros FA, Susanna R, Jr., Weinreb RN. Five rules to evaluate the optic disc and retinal nerve fiber layer for glaucoma. Optometry. 2005;76:661-8.
- Zangwill LM, Jain S, Racette L, Ernstrom KB, Bowd C, Medeiros FA, Sample PA, Weinreb RN. The effect of disc size and severity of disease on the diagnostic accuracy of the Heidelberg Retina Tomograph Glaucoma Probability Score. Invest Ophthalmol Vis Sci. 2007;48:2653-2660.
- Medeiros FA, Zangwill LM, Bowd C, Sample PA, Weinreb RN. Influence of disease severity and optic disc size on the diagnostic performance of imaging instruments in glaucoma. Invest Ophthalmol Vis Sci. 2006;47:1008-1015.
| Steven Mansberger, M.D., M.P.H. is Associate Scientist and Director of Ophthalmic Clinical Trials at Devers Eye Institute, Legacy Health System in Portland, Ore. He is also Director of Glaucoma Services at the Veteran's Administration Hospital and Affiliate Associate Professor of Ophthalmology and Public Health and Preventive Medicine at Oregon Health Science University. Christoper Bowd, Ph.D. is Associate Research Scientist at the Hamilton Glaucoma Center, Department of Ophthalmology, University of California, San Diego in La Jolla, Calif. His research interests include development and evaluation of optical imaging techniques for the early detection and monitoring of glaucoma, and machine learning classifier analysis of imaging and psychophysical testing data. |








