Confirming a Questionable Glaucoma Diagnosis
Here's how various capabilities of Cirrus HD-OCT helped develop an accurate treatment plan.

|

|
By Iqbal K. Ahmed, MD, FRCSC, and Jennifer Calafati, MD
A 64-year-old Caucasian man was referred for an assessment of suspicious-looking optic discs and borderline intraocular pressures (IOPs). The patient had no visual complaints but was slightly myopic. He had hypertension and diabetes and was taking medications for both conditions. He had no known family history of significant ocular diseases.
Ophthalmic Assessment
The patient's visual acuity was 20/25 in both eyes, and he had a mild myopic (–0.75D) correction. His IOP was 21 mm Hg in the right eye and 20 mm Hg in the left eye. Central corneal thickness (CCT) was 550 microns in the right eye and 554 microns in the left eye.
Optic disc examination of the right eye showed some suspicious cupping with early inferior and superior thinning of the neuroretinal rim. The left optic disc seemed to have a normal inferior rim, although it appeared there might be superior neuroretinal rim thinning. Clinical assessment of the retinal nerve fiber layer (RNFL) in both eyes revealed no obvious defects.
Humphrey automated perimetry 24-2 showed that both eyes had significant fixation losses with low reliability. We found no obvious visual field defects in either eye. Repeated automated perimetry showed variable reliability and was within normal limits.
Our standard ophthalmic workup revealed suspicious optic discs, particularly in the right eye, with borderline IOPs and normal CCTs. Visual fields, although not entirely reliable with multiple testing, was within normal limits. The question was, "Does this patient have glaucoma or not?"
Cirrus HD-OCT Difference
Cirrus HD-OCT provides rapid high-resolution scanning of the entire retina, retinal pigment epithelium and choroid. It's an important tool in glaucoma diagnostic imaging because it measures the thickness and quality of the peripapillary RNFL, possibly where the earliest glaucomatous changes occur. Emerging studies support the use of RNFL imaging as potentially more sensitive and specific than disc imaging for early glaucoma.1
Unlike time domain OCT, the Cirrus HD-OCT platform, which is based on spectral domain technology, collects large amounts of data over a large area of the optic disk with a single scan. Instead of performing a circular scan around the optic disk, Cirrus HD-OCT captures an optic disk cube, or a 200 A-scan × 200 B-scan area (6 mm × 6 mm) around the disc, thereby acquiring data from the peripapillary region as well as from the optic disk itself (Figure 1). You can measure over 42 million points within this area, which is an incredible amount of important data.
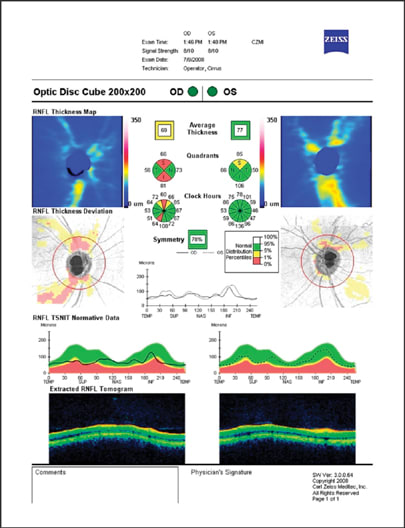
Figure 1. Cirrus HD-OCT captures an optic disk cube, or a 200 A-scan × 200 B-scan area (6 mm × 6 mm) around the disk, thereby acquiring data from the perpapillary region as well as from the optic disk itself.
RNFL Thickness Values, TSNIT Profile
Average RNFL thickness indicates a patient's overall RNFL health. The mean value for RNFL thickness in the general population is 92.9 +/- 9.4 microns. Typically, a normal, nonglaucomatous eye has an RNFL thickness of 80 microns or greater. An eye with an average RNFL thickness of 70 to 79 is suspicious for glaucoma. An average thickness of 60 to 69 is seen in less than 5% of the normal population and implies glaucoma.
The average RNFL thickness in our patient's left eye fell within normal limits. The average RNFL thickness of the right eye was 69 microns — below the fifth percentile of the normal population. The symmetry analysis between the RNFL of the right eye and left eye was 78%, which is within the normal range but is below the established mean of 88.6%. Asymmetry of RNFL thickness can be a useful finding in the diagnosis of glaucoma.
Since most glaucoma diagnoses present with localized defects, the quadrant analysis of Cirrus HD-OCT can be very helpful. When we analyzed each quadrant of our patient, it was clear that he had superior and inferior RNFL loss in the right eye that was outside normal limits. His RNFL thickness in these quadrants was in the red zone, indicating that his RNFL was in the lowest 1% of age-matched controls. Surprisingly, we found there was also some possible RNFL loss superiorly in his left eye, as indicated in the yellow zone (Figure 2).

Figure 2. The patient's RNFL thickness OD in this quadrant/clock hours analysis was in the red zone, indicating that his RNFL was in the lowest 1% of age-matched controls.
These results were also demonstrated in the longitudinal TSNIT thickness profile compared to normative data. The profile showed flattening of the superior and inferotemporal RNFL bundles in the right eye as well as subtle flattening of the superior RNFL bundle in the left eye. The asymmetry was also noted when we compared both TSNIT profiles.
Deviation from Normal Maps
The RNFL thickness maps and deviation maps are an innovation of the Cirrus platform that provides a transverse assessment of RNFL thickness across the 200 × 200 optic disk cube. Because of the rapid and precise volumetric imaging over this large area, we're able to get a birds eye view of the optic disk and peripapillary region.
The RNFL thickness map shows RNFL thickness along a color scale from areas of thinner RNFL in blue to areas of very thick RNFL in red. In our patient, the RNFL thickness and deviation maps corroborate the thickness values and TSNIT findings. The thickness map of the left eye shows some reduction of the typical yellow/orange RNFL peaks superiorly, while the right eye shows large areas of blue at the vertical RNFL poles (Figure 3).

Figure 3. The RNFL thickness map of the left eye shows some reduction of the typical yellow/orange RNFL peaks superiorly, while the right eye shows large areas of blue at the vertical RNFL poles.
The RNFL deviation map shows the superior and inferior loss along the RNFL bundles in the right eye, and the superior loss along the RNFL bundles in the left eye. Interestingly, the map also shows some early inferotemporal loss along the RNFL bundles about a disk diameter away from the disk in the left eye, although the disk itself looks untouched inferiorly (Figure 4). This specific finding likely would have been missed if we assessed the disk — clinically, with imaging or with peripapillary RNFL circle scanning — using other imaging technologies.

Figure 4. The RNFL deviation map shows the superior and inferior loss along the RNFL bundles in the right eye, and the superior loss along the RNFL bundles in the left eye.
Glaucoma or Not?
Although our clinical exam and early ancillary testing in this patient led to a possible diagnosis of glaucoma — at least in one eye — it was Cirrus HD-OCT that helped us make the diagnosis for both eyes. Cirrus HD-OCT illustrated the extent of glaucomatous damage by providing crystal clear views of RNFL thinning. Specifically, the Cirrus confirmed that the patient's right eye had greater RNFL loss and deviation from the norm than the left eye. Based on these findings, we diagnosed our patient with early open-angle glaucoma in both eyes. As a result of Cirrus HD-OCT technology and a solid diagnosis, we prescribed IOP-lowering medications in both eyes to slow the progression of optic nerve damage. OM
| Reference |
|---|
| 1. Medeiros FA, Vizzeri G, Zangwill LM, Alencar LM, Sample PA, Weinreb RN. Comparison of retinal nerve fiber layer and optic disc imaging for diagnosing glaucoma in patients suspected of having the disease. 2008. Ophthalmology. 2008;115:1340-1346. |








