My First 1,000 Advanced Surface Treatment Cases
I have differentiated my practice by appealing to safety-conscious patients.
BY ROBERT J. MITCHELL, M.D., F.R.C.S.C.
Like most refractive surgeons, my approach to laser refractive surgery has evolved greatly over the years. In the early ‘90s, I performed LASIK on all my patients and considered it a vast improvement over PRK. By 1999, although I was still happy with LASIK, I was using a newer surface ablation technique (laser epithelial keratomileusis [LASEK]) for the 30% of cases in which I had concerns about dry eye, ectasia or other problems that might be complicated by a lamellar flap.
I began performing Epi-LASIK with the Moria (Antony, France) Epi-K epithelial separator in 2005; immediately I recognized it as the innovation I’d been looking for in surface ablation. At first, I was replacing the epithelial flap created by the Epi-K. Then, in one case where the patient’s epithelial flap was lost, I noticed that his vision recovered more rapidly than usual and with less pain. I also heard that some surface ablation advocates were deliberately discarding the Epi-LASIK flap, and I gradually switched to that method myself.
In this article, I will describe this technique, dubbed Advanced Surface Treatment (AST), and explain why I now use it for all my laser vision correction cases.
Motivation for a Change
Today, my practice is 100% AST. The decision to stop performing lamellar surgery had nothing to do with visual outcomes. My LASIK outcomes were good and complications were rare, but the time and stress involved in dealing with even 1 LASIK patient in 20 with a complication made surface ablation a very appealing alternative for me.
I don’t think anyone would disagree that AST is safer than LASIK. It offers a lower risk of ectasia, fewer serious complications and, I feel, better contrast sensitivity. In addition, AST doesn’t cause or worsen dry eye. In Calgary, where I practice, the environment is quite arid, making post- LASIK dry eye a major problem. Of the 10,000 or so patients on whom I have performed LASIK, 200 to 300 of them still require treatment for severe dry eye, a condition that was probably exacerbated by the laser procedure.
Vast Improvement Over PRK
Anyone who recalls the discomfort and long healing times patients experienced with PRK will be pleasantly surprised to see the difference with AST. The Moria Epi-K makes a smooth, regular bed for the ablation, and with no affected cells covering the treatment area, the cornea quickly re-epithelializes. Whereas PRK was manual and rough, AST is automated and smooth, and I have had no trouble explaining this distinction to patients.
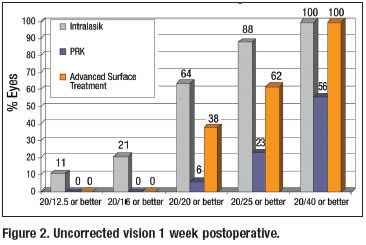
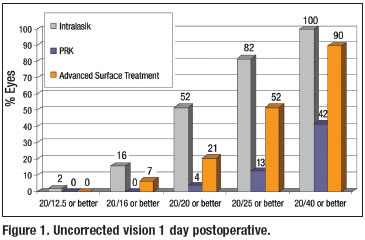
Visual recovery after AST is slower than with LASIK, but much faster than with PRK. At the 2006 European Society of Cataract and Refractive Surgeons meeting, Stephen G. Slade, M.D., and Daniel S. Durrie, M.D., presented a contralateral eye study comparing their results for alcohol-assisted PRK and LASIK. For both groups, they used the latest Alcon CustomCornea wavefront technology (Fort Worth, Texas). The LASIK flaps were created with the 60-kHz IntraLase femtosecond laser (IntraLase Corp., Irvine, Calif.). Not surprisingly, the LASIK early postoperative VA results were far superior to the PRK results, with 52% of LASIK (IntraLase) eyes achieving 20/20 on the first postoperative day, compared to only 4% of PRK eyes. At one week, 64% of LASIK eyes were seeing 20/20, compared to about 6% of PRK eyes.
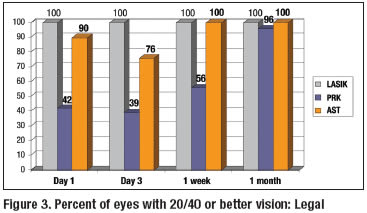
When I compare my latest AST results, using the Epi-K and the Carl Zeiss Meditec MEL 80 laser (Dublin, Calif.), to the Slade-Durrie data, one can see that while the early VA results fall short of LASIK, the 20/20 rates for AST are five times better than PRK on the first postop day (Figure 1) and six times better than PRK at 1 week postop (Figure 2). The percentage of AST patients who achieve 20/40 or better vision — the legal threshold for driving — is 90% at one day and 100% at 1 week, very similar to the 20/40 rates for LASIK and far better than the 20/40 rates for PRK (Figure 3).
With AST, my patients have very good early postoperative vision compared to previous surface ablation techniques. The minor blurriness in the initial postop period does not impede their daily activities, and it is a tradeoff that my patients accept for the increased safety of AST.
Establishing a Niche
In addition to providing clinical benefits, becoming an all-AST practice has distinguished us in the marketplace. The concept of “no-cut laser vision correction” is appealing to patients. Most visit at least a couple of different refractive surgery practices and, once they understand their options, are drawn to us because of the safety of AST. Although two competitors use IntraLase, I do not believe we have lost any patients to those practices. The safety-conscious patient who likes the idea of all-laser LASIK is going to like no-cut laser vision correction even better. We can also treat a wider range of patients than our competitors, because ablation depth and other factors do not eliminate as many candidates.
The Right Pain Regimen
Refining the postop pain regimen is important with any surface procedure. At first, our regimen included many different elements to maximize patient comfort. We put on a bandage contact lens and prescribed a steroid, NSAID, fluoroquinolone, diluted proparacaine “comfort drops” and frequent tears. We also gave the patients oral vitamin C, ibuprofen and gabapentin, as needed.
Today, however, we have a much more streamlined postoperative regimen that has been significantly more effective. The major difference is that we switched to using an Acuvue Oasys (Vistakon) bandage contact lens. I noticed a tremendous improvement in patient comfort with this contact lens. I have heard that others are soaking the lens first in balanced salt solution or in preservative-free anesthetic before placing it on the eye.
We began eliminating elements of our postoperative regimen one by one. When it comes to any post-surgical topical medication, less is more, in my opinion. We eventually dropped the comfort drops and the NSAID altogether, reduced the frequency of the steroid, and switched from preserved Refresh (Allergan, Irvine, Calif.) tears to nonpreserved Bion Tears (Alcon Laboratories). I instruct patients to use tears frequently and to keep their eyes closed as much as possible during the 2 days following surgery.
Eliminating the proparacaine and the NSAID, both of which retard healing, has shaved about 1 day off the postop recovery period. Patients who are fully compliant with my instructions generally have good visual recovery in 3 days, when I remove the bandage lens. Those who don’t use tears as frequently may take 5 days to fully recover.
The need for oral pain medication has been almost eliminated as well. With the prior regimen, about one-third of my patients experienced at least mild discomfort, and approximately 10% reported the pain was “severe.” Once we began discarding the flap and switched to the new bandage contact lens and artificial tears, only about 5% to 10% have any discomfort at all, and none of them have experienced severe pain or needed to take the gabapentin.
Outcomes From 1,000 Cases
I recently conducted a retrospective analysis of my first 1,000 myopic AST procedures, performed over the past 18 months. Preoperative myopia ranged from -1.5 D to -8 D. Postoperatively, all were within 0.5 D of emmetropia. Mean BCVA was 20/20 preoperatively, with no change postop. The enhancement rate in these 1,000 patients was 6%. As might be expected, it was lower (2%) in patients with low myopia and about 8% in those with >3 D of refractive error.
There have been no infections or other serious complications. Seven percent of patients have experienced mild pain, none severe. About 8% had somewhat delayed healing, up to 6 days. This is a long way from the LASIK days of diffuse lamellar keratitis, basement membrane dystrophy, flap complications and dry eye. The results in hyperopic eyes are just as good, if not better.
In summary, with AST, I have been able to achieve excellent results and quick visual recovery, relative to PRK. The procedure is safer than LASIK and effectively painless, now that I have settled on the optimal postoperative management regimen. The “no cut” approach holds such tremendous appeal for patients that shifting to 100% AST has been a practice growth engine.
Robert J. Mitchell, M.D., F.R.C.S.C., is clinical assistant professor at the University of Calgary and Director of Mitchell Eye Centre in Calgary, Alberta. Contact him at (403) 258-1773 or drm@mitchelleyecentre.com.








