The Case for Earlier Trabeculoplasty
This intervention can reduce patients’ need for medications.
BY L. JAY KATZ, M. D.
Patient adherence to medication is an issue pertinent to any condition, but it is particularly critical in a chronic condition like glaucoma, which, in early to moderate stages, has no symptoms. In this article, I will discuss adherence to medications, and make the case for the treatment alternative of laser trabeculoplasty and why physicians might want to consider this option earlier rather than later in a patient’s treatment plan.
Adherence Issues
When dealing with glaucoma cases, patients’ non-adherence with medical therapy may ultimately be devastating to their vision and quality of life. It is our goal to maintain their quality of life by preserving their vision in a way that works best for them and their lifestyle. Putting certain patients on multiple eyedrops may effectively save their vision, but may not be what is best for maintaining their quality of life due to potential side effects.
Patients must be alerted to the possibility of side effects. What physicians must recognize is that side effects may lead to poor patient adherence. For example, a patient who knows that he will experience red eyes as a result of his eyedrops may choose not to use them at certain times.
Furthermore, cost issues may have an effect on adherence rates, because some patients may not be able to afford medications. Multiple medications pose even more of a challenge. Adding more eyedrops with more copays and other out-of-pocket expenses can discourage some patients from complying with their treatment schedule. Other factors that can attribute to poor adherence to medications include the need for assistance in administrating the medications, forgetfulness, physical infirmity and arthritis, as well as complexity of the dosing schedule.
Alternatives to Medications
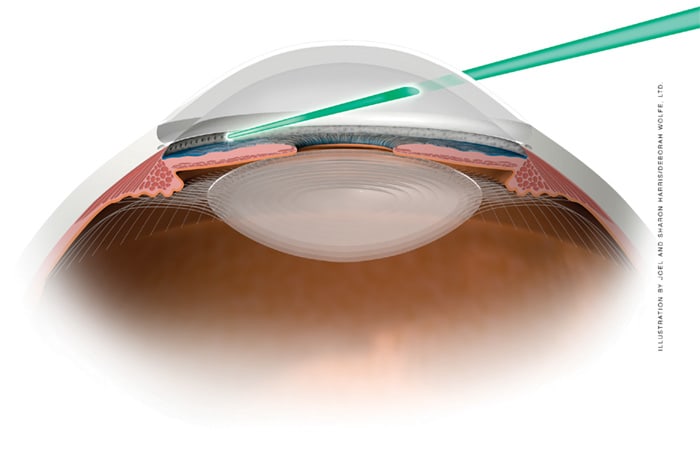
Surgical intervention in glaucoma, such as laser trabeculoplasty (Figure 1) or trabeculectomy, has customarily been considered an alternative only after:
► Drugs have failed to sufficiently lower IOP, or;
► The patient is not sufficiently adherent to his or her prescribed medications.
However, I contend that patients might benefit from laser trabeculoplasty or surgery as first-line therapy.
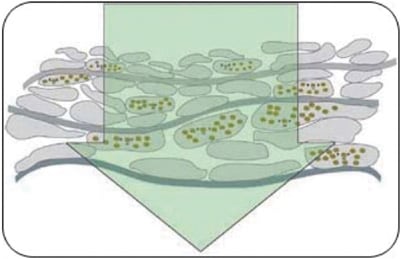
Figure 1. Laser trabeculoplasty: Representation of laser beam penetrating trabecular meshwork.

Figure 2. Trabeculum meshwork tissue after ALT.
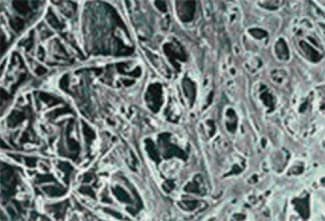
Figure 3. Trabeculum meshwork tissue after SLT.
Previously, the standard treatment pattern would be to exhaust all medication options before considering laser or surgery. This meant that patients could be prescribed up to four or five daily medications before other treatments were even considered. However, recent research suggests that laser or incision surgery may be appropriate earlier in the treatment paradigm for certain patients. Incisional surgeries such as trabeculectomy have also been suggested as a valid first-line therapy that works just as well as medications.1 However, most physicians do not recommend surgery as first-line therapy because of the risk of intra- and postoperative complications (such as intraoperative suprachoroidal hemorrhage, postoperative bleb infection and endophthalmitis). Serious complications are rare but do occur, which is why surgery is typically held in reserve for when other methods fail.
Introduced in the early 1970s, laser trabeculoplasty uses a laser to penetrate the trabecular meshwork (TM). The irradiation triggers biological and chemical mechanisms that together improve aqueous outflow in eyes with primary open-angle glaucoma or ocular hypertension.
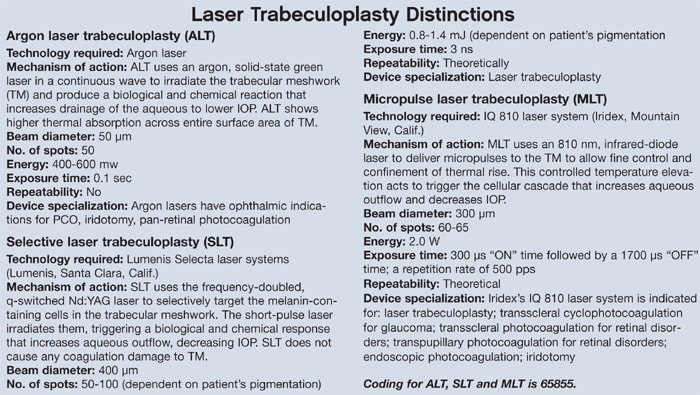
Argon laser treculoplasty (ALT) uses an argon laser applied in a continuous wave to induce photocoagulation necrosis of TM cells. The laser beam is applied over approximately 50 spots, covering an area of about 200 μm.
Selective laser trabeculoplasty (SLT) uses a 532 nm Q-switched, frequency-doubled Nd: YAG laser to emit short pulses that target pigmented melanin cells. The ability to burn the TM selectively means that SLT can precipitate the biological and chemical mechanisms needed to improve aqueous outflow, but without damaging adjacent, non-pigmented cells (Figures 2 and 3). Like ALT, SLT is applied over approximately 50 spots at 180°, but SLT has a larger beam diameter, so it treats a larger area of the TM (approximately 400 μm) and eliminates the need for fine focusing (Figure 4).
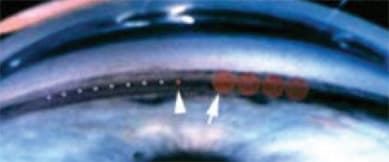
Figure 4. ALT spot size (left arrow) vs. SLT spot size (right arrow) in trabecular meshwork.
Laser trabeculoplasty has been gaining more data supporting first-line therapy use. Studies such as the Glaucoma Laser Trial (GLT) compared ALT with topical medical therapy in a stepped regimen. The researchers noted that ALT could be effective therapy without any medications in certain patients.2
More recently it has been suggested that SLT be used as a first-line therapy. McIlraith et al. concluded that SLT and latanoprost (Xalatan, Pfizer) are "equally efficacious" in reducing IOP in patients with newly diagnosed open-angle glaucoma and ocular hypertension.3 Similar findings have been reported by others, supporting SLT as an acceptable and efficacious option for first-line treatment.4,5
In my experience, using laser trabeculoplasty, particularly SLT, as a first-line treatment over medications often offers tangible, direct benefits: The burden of having to remember taking mediations can be eliminated or reduced, and annoying side effects, as well as cost issues, are alleviated.
While there is currently little information regarding retreatment, early research suggests that SLT may be repeatable in certain patients with good results.6 Additionally, data show that SLT results in a more intact trabecular meshwork than ALT, and may therefore be a repeatable treatment.7 Laser trabeculoplasty for our patients does not expose them to the side effects associated with medications or complications associated with incision surgery.
Choosing a Treatment Option
Many physicians call managing glaucoma an "art." Customizing a treatment course for a patient depends on understanding the patient’s preferences, history and physical examination. A conversation with patients about their options helps the physician determine what treatment will work best with that patient’s lifestyle, expectations and glaucoma stage. Patients may be most comfortable starting off with medications, but, depending on their lifestyles, some may willingly elect laser or, on rare occasions, incision surgery if they feel it will control their IOP the best. Overall, when choosing a method of treatment, we aim to keep patients healthy and independent. Technology today has provided us with many options to achieve that goal.
In my practice, we explain to patients that laser trabeculoplasty today is reasonably safe and performed in the office. Patients tend to be more at ease with in-office procedures. For patients who are at high risk for non-adherence, such as those who may be forgetful about taking medications, experience tremors and/or live alone, I feel it is obligatory to offer options such as laser trabeculoplasty.
Think Outside the Box
Adherence with medical therapy in glaucoma patients is a constant concern when it is the physician’s goal to balance saving vision and maintaining a high quality of life. In my opinion, alternative treatments, such as laser trabeculoplasty and, on occasion, even incisional surgery, should be considered earlier in the treatment paradigm. Once the patient is fully evaluated, it should become clearer what the options are for treating the patient. For example, someone who has an extremely elevated IOP probably would not be an ideal candidate for laser trabeculoplasty since an immediate IOP drop is not likely. As adjunctive therapy, laser trabeculoplasty appears to have less of an effect when used following failure with multiple medications.3 However, introducing the concept of laser trabeculoplasty earlier in the treatment paradigm has given physicians the opportunity to help certain patients stabilize their glaucoma. OM
References
1. Lichter PR, Musch DC, Gillespie BW, et al; CIGTS Study Group. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study (CIGTS) comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108:1943-1953.
2. Glaucoma Laser Trial Research Group. The Glaucoma Laser Trial, II: Results of argon laser trabeculoplasty versus topical medicines. Ophthalmology. 1990;97:1403-1413.
3. McIlraith I, Strasfeld M, Colev G, Hutnick CM. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma. 2006;15:124-130.
4. Melamed S, Ben Simon GJ, Levkovitch-Verbin H. Selective laser trabeculoplasty as primary treatment for open-angle glaucoma. Arch Ophthalmol. 2003;121:957-960.
5. Nagar M, Oqunyomade A, O’Brart DP, Howes F, Marshall J. A randomized, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol. 2005;89:1413-1417.
6. Nagar M. SLT — Effect of Enhancement and Repeatability on IOP Poster presented at: Annual meeting of the American Academy of Ophthalmology; Nov. 2006; Las Vegas, Nev.
7. Lai J, Bournias, TE. Repeatability of selective laser trabeculoplasty (SLT). Presented at: Association for Research in Vision and Ophthalmology; May 2005; Fort Lauderdale, Fla.
| L. Jay Katz, M.D., is the codirector of the glaucoma service at Wills Eye Hospital in Philadelphia. He is an investigator for SLT/Lumenis, but has no financial interest in any of the products mentioned in this article. E-mail him at ljk22222@aol.com. |

|








