How to Correct Astigmatism In the Cataract Patient

By Steven J. Dell, M.D.
A veteran surgeon describes his techniques.
The main focus of a typical residency program is to acquire the surgical skills necessary to restore visual function in cataract patients. But as you make the transition from residency training to private practice, your focus will shift from simply restoring vision to delivering the best, uncorrected visual acuity. This requires addressing not only the spherical component of the refractive error, but also minimizing residual corneal astigmatism.
In this article, I’ll discuss the techniques I use to correct various degrees of astigmatism after cataract surgery, how I identify the right candidates for these procedures and the pros and cons of each.
High Expectations
Cataract patients today assume that living independent of spectacles is the normal postoperative result. This expectation probably stems from the many marketing messages touting laser vision correction. However, freedom from spectacles is possible only if the total refractive error — including astigmatism — is corrected.
Choosing the Best Procedure
In my practice, about 60% of cataract patients choose astigmatism-reduction procedures, such as limbal relaxing incisions (LRIs), laser vision correction (LVC), on-axis cataract incision and toric IOLs. I perform LRIs or LVC on most patients. A smaller number of patients do well simply with on-axis cataract incisions.
The procedure you choose depends on the amount of astigmatism the patient has. You can generally treat up to approximately 2.50D to 3.00D of astigmatism effectively with LRIs. For amounts higher than 3.00D, LVC generally is required. Toric IOLs can correct similar levels of astigmatism, but in the United States, the only two available toric IOLs are monofocal lenses. As a result, the use of toric IOLs to correct astigmatism is limited to patients who simply want good uncorrected distance vision. LRIs or LVC are most commonly used for correcting corneal astigmatism in patients interested in multifocals or accommodating technology.
For patients with a minimum amount of astigmatism, a 4.0-mm cataract incision placed on the steepest axis can achieve about 0.50D of flattening. Advantages include no extra cost to the patient, no additional instrumentation for you and no need for a second procedure. On the other hand, you need to be aware that incisions larger than 4.0 mm can increase the risk of wound leaks, the need for sutures and the possibility of endophthalmitis.
Best Candidates for LRIs
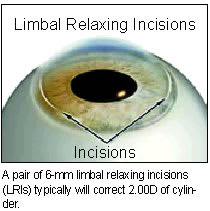
I tend to reserve LRIs for patients who want to reduce their dependence on spectacles and who have 0.60D or more of astigmatism. A single LRI with a 6-mm cord length and 550 micron depth can correct about 1.00D of cylinder, while a pair of 6-mm incisions typically will correct 2.00D of cylinder. I’ve been able to achieve 2.50D and sometimes 3.00D of flattening with longer incisions. I place LRIs on the steepest meridian, near the limbus at the 9.0-mm to 11.0-mm optical zones.
What’s important to remember is that you’re treating corneal cylinder not refractive cylinder with LRIs performed at the time of cataract surgery. The lenticular component of the astigmatism will be removed along with the lens. Preoperative topography is a prerequisite to LRIs, as is careful attention to incision depth and correct axis placement. The key is to maintain appropriate orientation throughout surgery. There are several instruments, such as the Dell Astig-
matism Marker (Rhein Medical), that can help you place the incisions in the correct meridian.

Pros and Cons of LRIs
LRIs have several advantages. The additional time it takes to do them and the cost are negligible. There’s virtually no learning curve, and you can perform them during cataract surgery, which reduces healing time and the risk associated with a secondary
procedure. Another perk: diamond knives preset to the appropriate depth of 500 µm to 600 µm are available. This eliminates the need for corneal pachymetry, which requires more time and equipment.
One of the drawbacks of LRIs is that they’re less precise and predictable than LVC because — as with all procedures requiring an incision — the outcome depends on wound healing. In addition, LRIs can exacerbate dry eye syndrome. Whenever you perform an LRI, you sever corneal nerves, which can aggravate dry eyes. And when you perform a pair of LRIs, essentially you denervate a large segment of the cornea and render it neurotrophic. To reduce the risk of this complication and enhance the healing process, you can administer artificial tears and/or topical cyclosporine (Restasis) to patients preoperatively.
Many of the contraindications associated with LVC, such as forme fruste keratoconus or pellucid marginal degeneration, also may be linked to LRIs. So tread carefully when making these incisions in unstable and irregular corneas.
Laser Vision Correction
LVC enhancement is the best option for patients with more than 3.00D of astigmatism. This procedure offers the highest level of precision because it achieves the intended amount of astigmatism correction — especially when you use a laser system that incorporates iris registration. Iris registration compensates for cyclotorsional misalignment, and
it’s particularly important in high-cylinder ablations.
Surgical Fees
When it comes to surgical fees, in my practice, we charge patients a reasonable fee for LRIs or LVC. We provide LVC enhancements at a reduced rate for our patients who are already paying a premium for presbyopic IOLs. Other practices bundle the cost of LVC with the fee for their presbyopic IOLs. Patients receiving standard IOLs also can have their astigmatism corrected with LVC. But, in my practice, they must pay the full price for this elective procedure.
Toric IOLs
Toric IOLs correct sphere and cylinder without additional incisions, but — unlike multifocal or accommodating lenses — they don’t provide a range of vision, so spectacle independence at near isn’t an option.
Toric IOLs usually have to be specially ordered and are more expensive for the facility, but the costs associated with diagnosing and planning the surgery can be passed along to the patient, according to a recent clarification of Medicare regulations.
As is the case with LRIs, misalignment is a major concern with toric IOLs, although templates are available to ensure placement on the proper meridian. When considering a toric IOL, focus your preoperative evaluation on ruling out anything that can influence a shift in the lens position, such as capsular rupture or zonular dehiscence. Misalignment during surgery can increase astigmatism. Postoperative rotation also is possible, which could require surgical repositioning of the lens.
Focusing on Two Aspects
Modern cataract surgery involves two aspects of vision improvement: replacing an opacified lens and correcting any residual refractive error. Today’s savvy cataract patients are well aware of the many procedures that can make them less dependent on spectacles, and they’ll expect you to offer what’s right for them. So learn all you can about correcting surgically-induced or residual astigmatism following cataract surgery during residency training. When it’s time to move into private practice, you’ll be prepared to meet the higher demands of your patients.
Steven J. Dell, M.D., is a clinical instructor in ophthalmology at Tulane University in New Orleans and director of refractive and corneal surgery at Texan Eye Care in Austin, Texas.








