Fine Points for Explanting IOLs
Perspectives on conditions and technique.
BY HARRY B. GRABOW, M.D.
When a surgeon must explant an IOL, myriad issues are involved: indications for explantation must be considered, and risks vs. benefits must be weighted, and preoperative and intraoperative planning must be executed to ensure a successful outcome. I will review these issues in this article.
Indications for IOL Explantation
■ Intraoperative. The surgeon may need to remove an IOL at the time of primary implantation if it is damaged during insertion, if it is discovered to be the incorrect power, or if damage to the ocular tissues occurs during insertion, rendering the primary IOL unstable in the eye. Damage to an IOL can occur to a haptic or the optic. Haptic damage includes a bent or avulsed haptic, in the case of a looped or three-piece IOL, or a torn or avulsed portion of a plate-haptic in the case of a single-piece silicone (Figure 1) or Collamer (Staar, Monrovia, Calif.) IOL. If it is determined that the haptic damage renders the IOL unstable or decentered, the surgeon should remove and replace the IOL.
Damage to the capsule, particularly a posterior tear that occurs during primary IOL implantation, may require primary IOL removal and replacement with an IOL in a different location.
■ Postoperative. In the early postop period, the surgeon may remove an IOL (and exchange it) if there is an undesired refractive result, and the patient prefers neither a corneal refractive procedure nor a “piggy-back” IOL. In these situations, it is easier and safer to remove an IOL from the capsular bag earlier rather than later when fibrotic contracture and scarring could make IOL removal risky for zonulodialysis.
Another indication for early IOL removal (and exchange), albeit extremely rare, would be intolerable negative dysphotopsia in a first eye, usually associated with a square-edged acrylic IOL, wherein the patient refuses to have the second eye done until the “disabling” temporal shadow is gone. Often, however, these symptoms abate with time, requiring no surgical intervention. In such cases, the replacement IOL and the second-eye IOL are round-edged silicone or collagen IOLs.
The most common late indication for IOL removal (and replacement) is symptomatic malposition,1 such as decentration (Figure 2), subluxation (Figure 3), or total dislocation (Figure 4). IOL malposition can be the result of asymmetric fibrotic contracture of the capsule, an eccentric capsulorrhexis (Figure 5), asymmetric IOL placement with one haptic in the bag and one in the sulcus, following Nd:YAG laser posterior capsulotomy, or the result of trauma. With the increasing use of presbyopic IOLs, IOL position is even more critical. Multifocal IOLs with only minor decentration can be symptomatic requiring removal. An accommodative IOL, particularly the one plate-haptic model (crystalens, eyeonics, Aliso Viejo, Calif.) has demonstrated a unique positional malfunction wherein capsular contraction can cause long-axis compression with asymmetric folding at the haptic-optic junction. This results in optic tilting with up to 3.0 D of pseudophakic astigmatism (Figure 6). This unique constellation has been called “Z-syndrome” due to the shape of the distorted IOL and can necessitate IOL removal. If the surgeon finds at the time of explantation that the IOL is fixed in the capsular fornices, haptic amputation may be necessary with removal of the optic only.
Another indication for late IOL removal due to malposition is partial or total zonulodialysis, as can occur in Marfan’s syndrome, pseudoexfoliation,2 excessive capsular contraction due to fibrosis or following ocular trauma. Even if a simple capsular tension ring (CTR) had been placed at initial surgery, zonulodialysis can occur and progress, resulting in partial IOL/capsular subluxation (Figure 7) or even total dislocation (Figure 8). In these cases, IOL and CTR removal is an option. If this is elected, once the complex is elevated into the anterior chamber and the pupil constricted, the capsule can be incised, separating the IOL from the CTR. Each component can then be removed separately through a small incision. An alternative to removal of the components is to reposition the complex in the sulcus by suture fixation of the CTR and/or IOL haptics to the sclera with 9-0 Prolene3,4 (Figure 9), or by suture fixation to the posterior iris.5



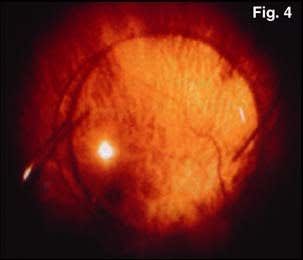
Figure 1. silicone plate-haptic IOLs that should be removed.
Figure 2. Postoperative fibrotic intracapsular decentration of three-piece IOL.
Figure 3. Plate-haptic silicone IOL subluxation.
Figure 4. Total posterior IOL dislocation.
Handling Complications
A rare late IOL complication is optic opacification. This can occur spontaneously in both hydrophobic and hydrophilic IOLs, and can occur as a result of excessive central optic pitting during Nd:YAG laser posterior capsulotomy.6,7 When severe enough to be symptomatic, IOL removal/replacement is indicated.
An eye that has an anterior chamber IOL, be it phakic or aphakic, can develop symptomatic pupillary ovalization (Figure 10), iritis and glaucoma. In addition, IOLs in the anterior chamber may cause focal or generalized loss of corneal endothelial cells that may develop into corneal edema. In this case, IOL removal may be indicated, with or without penetrating keratopolasty or Descemet’s stripping automated endothelial keratoplasty, with IOL replacement in the posterior chamber (usually requiring suturing to the posterior surface of the iris or the sclera). A phakic posterior-chamber IOL can decenter, especially if sized too small or if sharp edges or corners exist that can damage zonular fiber attachments, and can also cause a symptomatic anterior subcapsular cataract (Figure 11). Any of these adverse effects could necessitate phakic IOL removal.
Techniques of IOL Removal
■ Intraoperative. If a silicone IOL requires removal at the time of implantation, it can be done through the original incision after sectioning to “incision-size” pieces. The surgeon can perform this safely using a dispersive viscoelastic to protect both the corneal endothelium and the capsule. Several instruments are available for this purpose, including scissors of different types. A second method of removing a three-piece silicone IOL is by partially bisecting the optic only halfway to its center,8 and then removing the IOL by pulling the bisected hemi-optic through the incision. The IOL will either come out in one piece if rotated when the optic center reaches the incision, or the hemisection will continue to fracture with traction into two complete hemioptics. A similar method has been devised for plate-haptic silicone IOLs.9
If an acrylic IOL requires removal at the time of primary implantation, it can be repositioned in the anterior chamber, and, using a dispersive viscoelastic, either sectioned for removal in pieces or refolded and removed in one piece. Refolding usually requires a fulcrum instrument inserted through a paracentesis 180° away from the primary incision; then careful optic folding with folding forceps.
■ Postoperative. The techniques of removing IOLs postoperatively are no different than those intraoperatively; however, getting the IOL to a safe location for explantation often requires extra steps.
Late removal technique depends on the location of the IOL. IOLs that have been in the anterior chamber for a long period may have formed fibrous “cocoons” around the haptics, depending on the haptic design. This may be discernable preoperatively by gonioscopy. In these cases, the surgeon must rotate the IOL clockwise to dial the haptics out of their “cocoons” until the IOL is free of adhesions.
Forced rotation or attempt at simple linear extraction could result in iridodialysis and hyphema. Haptic amputation may be necessary if the IOL cannot be safely dialed. As these older IOLs are typically PMMA, incisions of 6.5 mm are usually required. It is helpful to place a dispersive viscoelastic both in front of and behind the IOL before any manipulation as most of these AC-IOLs have either an open posterior capsule or no capsule with no barrier to the vitreous.
IOLs attached to the front surface of the iris, such as the Artisan/Verisyse (AMO, Santa Ana, Calif.), must be disenclavated before removal. This requires stabilizing the IOL with forceps and then depressing the enclavated iris tissue at each “claw.” If the IOL is PMMA, a 6-mm incision is required; if the IOL is the foldable version (Artiflex/Veriflex, Ophtec), a smaller incision of 4 mm may be used.
Although IOLs that are fixated in the pupil have not been implanted for more than 20 years, there may be a few of these remaining. Chances are if they’ve been in these eyes that long, they have caused no problems. However, all of these were PMMA, some following intracapsular extraction (ICCE), such as the Copeland lens, and some following extracapsular extraction (ECCE), such as the Binkhorst 2-loop, Binkhorst 4-loop, Worst medallion lens and others. Removing these would require a 6.5-mm incision.
IOLs in the ciliary sulcus usually have no fibrotic attachment to the eye. They can usually be easily mobilized into the anterior chamber for explantation. By contrast, IOLs that have been in the capsular bag may have significant fibrotic adhesion between the anterior and posterior capsules. In addition, the anterior capsulorrhexis opening may have fibrotic contraction, phimosis, which can further restrict mobilization of an IOL from the capsular bag. In these cases, enlarging the continuous curvilinear capsulorrhexis (CCC) or radial relaxing capsulotomies may be necessary to allow safe passage of the optic. Hydrodissection and viscodissection can also facilitate separating fibrotic capsular adhesions. Take care to rotate the IOL, avoiding stress on the zonule, before attempting to elevate the IOL out of the bag. If the IOL cannot be mobilized within the capsule, haptic amputation may be necessary. In that case, one or both haptics may be left in the bag while only the optic is removed. Once the IOL is out of the bag, the surgeon can remove it through a small incision by sectioning if silicone, or by sectioning or folding if acrylic.




Figure 5. Fibrosis of the anterior capsule, eccentric capsulorrhexis, short-axis decentration of plate-haptic silicone IOL.
Figure 6. crystalens with anterior capsular fibrosis and phimosis, capsular contraction with “Z-syndrome” with 2 D of pseudophakic astigmatism.
Figure 7. Subluxation of capsule/IOL/CTR complex due to zonulodialysis.
Figure 8. Total dislocation of capsule/IOL/CTR complex following total zonulodialysis.
IOL Replacement
The replacement IOL implantation method and location are both dependent on the status of the ocular anatomy following IOL removal. If all is normal and there is an intact capsular bag, then the secondary implantation procedure is no different from the first; the IOL goes in the same location, usually the capsular bag.
If the posterior capsule was opened during primary surgery and if the tear is small, it is possible to convert it from an unstable tear that could extend to a stable posterior CCC. This is done by placing viscoelastic through the opening to tamponade the vitreous and using capsulorrhexis forceps. If a stable posterior CCC is made, there are several options for replacement IOL location. The primary IOL can be placed entirely within the bag, or the haptics can be placed in the bag with the optic captured through the posterior CCC. If the optic is placed through the posterior CCC, the IOL power should be adjusted 0.5 to 1.0 higher (more plus). If there is also a tear in the anterior capsule and a stable posterior CCC has been made, it is possible to place the haptics in the sulcus and the optic through the CCC.
If the bag has an unstable posterior opening but the anterior CCC is intact, then the replacement IOL can be located entirely in the posterior chamber. Alternately, if the anterior CCC is smaller than the diameter of the replacement IOL optic, the surgeon can place the haptics in the sulcus, while capturing the optic through the anterior CCC. If the optic is placed in the posterior chamber, the power is usually calculated to be 0.5 to1.0 less than the power of the bag lens.
If both the posterior and anterior capsules are unstable or absent, the surgeon can place the replacement IOL in the posterior or anterior chamber. If the surgeon prefers placement in the posterior chamber, the IOL may be sutured to the posterior surface of the iris or to the sclera. At present, 9-0 polypropylene is recommended for this procedure as it may have a life expectancy of greater than 10 years before hydrolysis (biodegradation) occurs. Additionally, an angle-fixated AC-IOL can be placed or an iris-fixated IOL, such as the Artisan/Verisyse varieties.

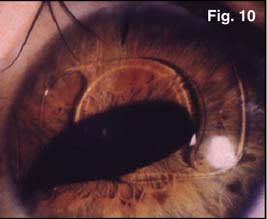

Figure 9. Scleral suture fixation of dislocated capsule/IOL/CTR complex.
Figure 10. Pupil ovalization from anterior chamber IOL.
Figure 11. Collamer phakic posterior chamber IOL withanterior subcapsular cataract.
References
1. Mamalis N. Complications of foldable intraocular lense requiring explantation or secondary intervention — 2006 update. Presented at the European Society of Cataract and Refractive Surgery Meeting; September 2006; Lisbon, Portugal.
2. Jehan, FS, Mamalis, N, Crandall, AS. Spontaneous late dislocation of intraocular lens within the capsular bag in pseudoexfoliation patients. Ophthalmology. 2001;108:1727–1731.
3. Chan, CC, Crandall, AS, Ahmed, IK. Ab externo scleral suture loop fixation for posterior chamber intraocular lens decentration: clinical results. J Cataract Refract Surg. 2006;32:121–128.
4. Hoffman, RS, Fine, IH, Packer, M. Scleral fixation without conjunctival dissection. J Cataract Refract Surg. 2006;32:1907–1912.
5. Condon, GP. Simplified small-incision peripheral iris fixation of an AcrySof intraocular lens in the absence of capsule support. J Cataract Refract Surg. 2003;29:1663–1667.
6. Werner, L, Apple, DJ, et al. Dense opacification of the optical component of a hydrophilic acrylic intraocular lens: a clinicopathological analysis of 9 explanted lenses. J Cataract Refract Surg. 2001;27:1485–1492.
7. Neuhann, IM, Werner L, et al. Late postoperative opacification of a hydrophyilic acrylic (hydrogel) intraocular lens: a clinicopathological analysis of 106 explants. Ophthalmology. 2004;111: 2094–2101.
8. Batlan, SJ, Dodick, JM. Explantation of a foldable silicone intraocular lens. Am J Ophthal. 1996;122: 270–272.
9. Osher, RH, Crisscross lensotomy: new explantation technique. J Cataract Refract Surg. 2006;32:386–388.
|









