office
The
Electronic Office
New
AAO initiative will promote full electronic workflow.
BY
FLORA LUM, M.D., AND LLOYD HILDEBRAND, M.D.
Today, in our ophthalmology practices, we have real-life problems with accessing data and integrating our systems. Paper charts have to be transported from one office to another. Two people cannot access the same chart at the same time. Systems are proprietary and when they are no longer supported, the data are lost. Images are missing, or have to be viewed at a separate workstation. The patient identifier information may be typed incorrectly at different points during the visit, so there needs to be reconciliation. The patient may not receive the right procedure and has to be rescheduled. Sometimes, an image may be put in the wrong patient chart.
The federal government is pressing for more open
and efficient flow of information. On Aug. 22, President Bush's Executive Order
mandated that federal agencies involved with health insurance use health information
technology (IT) standards to facilitate the rapid exchange of health information
(http://www.whitehouse.gov/news/releases/
2006/08/20060822.html). Secretary of
Health and Human Services Michael Leavitt is calling for the electronic sharing
of information using health IT standards so that one system can talk to one another
(http://www.hhs.gov/transparency/transparencybookletfinal.pdf).
The vision is full electronic workflow, eliminating the need for paper, film, or removable media to transfer information, and having patient care data anytime, anywhere. This article will describe this new initiative by the American Academy of Ophthalmology (AAO).
Full Interoperability of Data
Imagine the possibilities. What if you could see all the data gathered from all the different types of devices and instruments in your office at one computer workstation? What if some of the routine, tedious tasks that your office staff does could be automated? What if once a patient was registered, all the appropriate procedures would be scheduled with the accurate patient name and identifier information?
This vision will be realized at "The Electronic Office" at the AAO Annual Meeting, where different electronic health record (EHR) systems, imaging devices and other equipment will exchange information. This is called interoperability, the ability to share information electronically. Interoperability is only achieved if everyone adheres to the same standards, so that one system can talk to another system, sending information accurately, securely and efficiently. This is the "plug and play" approach, similar to how you can interchange any USB device into your computer.
The benefits of integrating systems for electronic workflow include accessibility, accuracy and automation. What are the specific benefits? They include:
► patients' images can be accessed anytime, anywhere
► patient identifier information is accurately attached to the correct image, so that there are no errors in matching
► steps in the clinical workflow are automated, thus reducing work and potential for human error
► patients' images can be displayed along with the patient record information, so that all the data needed to make clinical decisions is available
► the integrity of the data (images, words, numbers) is protected, i.e., the image quality should be the same at different display stations
► the electronic flow of information can be tracked from patient check-in through archive and billing
► every procedure performed can be tracked and reconciled with billing, so that every procedure is appropriately billed
► one interface is needed, not an interface that needs to be programmed individually for each separate medical device
► no need to worry about proprietary devices not being able to communicate with one another or about getting data from a legacy device
► being able to purchase new equipment without worries about lack of interfaces with existing equipment.
Success Across Medical Specialties
For several years, the AAO has sponsored standards-setting activities to foster more efficient clinical workflow and exchange of patient information. These have served as building blocks for making an EHR system more useful to ophthalmologists by allowing the understanding and aggregation of words (through a standardized terminology, known as Systematized Nomenclature of Medicine [SNOMED]), the exchange and display of images from different devices (through a standard for medical images, known as Digital Imaging and Communications [DICOM]), and the interchange and reporting of numbers from various devices such as a lensometer (through a standard for structured reports within DICOM and Health Level 7 [HL7] standards for patient registration and billing data). These building blocks for standardizing the communication of words, images and numbers serve as the foundation for electronic workflow, increasing efficiency and improving quality.
Several years of bringing vendors together in a neutral forum and soliciting buy-in on an open architecture and a common communication standard has resulted in "The Electronic Office — Integrating the Healthcare Enterprise (IHE) Eye Care." IHE is a broad medical initiative to provide a common framework for passing health information seamlessly (www.ihe.net). It is sponsored by healthcare professional associations, including the AAO, the Radiological Society of North America, the Healthcare Information and Management Society and the American College of Cardiology.
This integration has been highly effective in other medical specialties. DICOM and HL7 are well-accepted industry standards, and IHE has been a proven process for implementing these standards. In radiology, interoperability is a given, and IHE solutions are now available in hundreds of commercial radiology-related information systems and implemented in care sites around the world.
Beginning in January 2006, a dedicated group of ophthalmologists, IT professionals, Veterans Administration staff, and device and EHR vendors have worked on detailed specifications for enabling electronic workflow, known as the IHE Eye Care Technical Framework. All ophthalmic vendors were invited to join the group to build the specifications and participate in the demonstration this year. These specifications are in the public domain, and can be used by any vendor in product design. Ultimately, it saves manufacturers time and money, because they do not have to write interfaces for each piece of equipment. Proprietary solutions are discouraged, because these are not in the ophthalmologist purchasers' best interest, leading to legacy products and lost or unusable data.
|
|
|
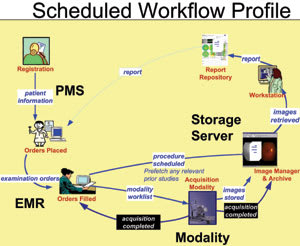
Figure. In the Eye Care Workflow, a patient is registered, the order for a procedure is placed, scheduled, performed, stored and ultimately retrieved by the ophthalmologist to view in order to make a diagnosis or a treatment decision. All of these actions are enabled through defined, structured messaging from one system to another. |
Focus Areas of the IHE
There are three focus areas of the IHE Technical Framework: Eye Care Scheduled Workflow, Billing Workflow and Evidence Documents Integration Profiles. These Integration profiles all address a real-life integration problem in eye care, and propose a solution, based on established standards such as DICOM and HL7.
The Eye Care Workflow Integration Profile deals with the following activities that are part of every patient visit: admit or register patients, order tests/images for patient, schedule procedures, create a worklist (or list of procedures that were ordered), monitor the status of procedures performed, create images, manage or keep track of images created and store and display images.
For example, a set of generic orders could be created for every patient, for routine procedures such as lensometry and autorefraction. Normally, these are performed by the staff, but not tracked with the patient identifier information. If they are part of the order set, then the worklists will have the patients listed with the correct identifier information. This alone could save staff time, and assure that the right information is tracked back with the right patient. Another step is notifying the technician when a test should be performed. Either by verbal order or through this workflow, the ophthalmologist places an order and the technician looks at the worklist to see exactly who needs which procedure to be performed. The creation and use of worklists saves time, because they can be used to automatically and accurately fill in information into images, eliminating the need for re-entry by the technician operating the device.
Within this system of interconnected devices and systems, several factors or elements are formally defined and have specific actions to perform.
■ Eye Care Workflow. In the Eye Care workflow (Figure), a patient-registration system (also known as an Admit, Discharge and Transfer [ADT] system) is responsible for patient demographic and encounter information. An order placer generates eyecare orders, such as fundus photos or visual field tests, and distributes these orders. An order-filler takes the eyecare order and coordinates with the image device to provide worklists of all the procedures being performed, and monitors the progress of the work being done. An acquisition modality is the imaging device or equipment (e.g., ultrasound equipment, fundus camera) that acquires the image and creates a DICOM object (so that it can be exchanged and displayed with other systems). An image manager/image archive keeps track of the images (stored as DICOM objects) and provides long-term storage. An image display provides the ability to see and browse patients' image studies.
| Electronic Office Showcase |
|
The
Electronic Office is located on the Exhibit Floor, Booth Number #4665. Companies
participating in this year's Electronic Office include three EHR systems and seven
medical devices. These include: Anka Systems, Canon, Carl Zeiss Meditec, Digital
Healthcare, Heidelberg Engineering, Kowa Optimed, Inc., MDOffice Inc., Medflow Inc.,
Nidek, Inc., Ophthalmic Imaging Systems, Ophthalmic Technologies Inc., Topcon Medical
Systems and VersaSuite. At the showcase, after initial check-in, order a procedure. Next, have an image taken (e.g., fundus camera, ultrasound, optical coherence tomography). Then, proceed to a workstation to view your image, along with your registration information. There will also be speakers and presentations to help participants understand more about the electronic workflow. There will also be three related sessions at the Technology Pavilion: ► Sunday, Nov. 12, 2:30 p.m. to 3:30 p.m.: "The Electronic Office is Here: Automation of Clinical Workflow from Patient Registration to Billing" ► Monday, Nov. 13, 11 a.m. to 12 p.m.: "Electronic Health Records Connecting with Imaging Devices: All the Patient Data at One Workstation" ► Tuesday, Nov. 14, 11a.m. to 12 p.m.: "Electronic Health Records, Electronic Workflow to Reduce Errors, Reconcile Billing and Incorporate Legacy Systems" |
In the future, image manager/image archive/image display products will be more involved in networking in ophthalmology. In a network, the devices will acquire the images, the image manager/archive products will store the images and evidence documents, and the image display will show this information on workstations. This is commonly done in radiology, where these are known as picture archiving and communication systems (PACS).
■ Charge-Posting Profile. This provides a solution for collecting and posting timely billable procedural details. The Charge-Posting Profile would work in the office as follows: The registration system would provide the billing system with the patient demographic information, accounts, insurance and guarantors. After a procedure has been completed, the acquisition modality or device would send the procedure code and the patient identifier information to the order filler. The order filler would map the procedure code to a CPT code. The order filler would notify the billing system that a billable procedure has been completed. The billing system and administrator would then perform any remaining steps to generate the appropriate bill. The benefits include: ensuring complete data, less staff resource requirements for billing reconciliation, reduces redundant data entry and maintains data integrity. The end result is that the billing system will receive more complete, timely and accurate data.
■ Evidence Document Profile. This profile
is intended for the incorporation of additional measurements and observations as
documents: creating, storing, retrieving and using these different documents as
a record of evidence.
Detailed information, such as reconstructed or derived images, measurements, post processing results, etc. could be made available as input in the generation of a clinical report to the ophthalmologist. Examples include: glaucoma progression analysis performed on visual field analyzers; retinal nerve fiber analysis performed on an optical coherence tomograph device, measurements on fundus images and corneal ablation planning based on corneal topography maps. These evidence documents can be transferred, stored, and retrieved just like images. This profile will be demonstrated at the 2007 Electronic Office Showcase.
Flora Lum, M.D., is policy director of Quality of Care and Knowledge Base Development at the American Academy of Ophthalmology. Lloyd Hildebrand, M.D., is chair of the AAO Medical Information Technology Committee. Dr. Lum can be e-mailed at flum@aao.org.