feature
Clinical
Use of Aspheric IOLs
Understanding
the physics of optics will help you improve patient outcomes with this technology.
BY UDAY DEVGAN, M.D., F.A.C.S.
In the current age of refractive cataract surgery, we measure the quality of vision in addition to the quantity of vision. The patient's image quality is as important as his Snellen acuity, particularly when we operate on patients with high expectations and high demands for their vision.
In the last few years the clinical use of aspheric IOLs has grown dramatically, with aspheric IOLs steadily gaining market share. Medicare has even awarded New Technology IOL (NTIOL) status to some aspheric IOLs, indicating their agreement that these lenses offer a significant benefit over their predecessors.
Understanding the concepts behind these new IOL designs is instrumental to their effective use. And since many cataract surgeons, like me, have forgotten the extensive physics of optics that were learned during residency, I have prepared a concise summary.

|
| Figure 1a. Spherical lenses have a constant curvature, as they are derived from spheres, which results in peripheral light rays being defocused. Figure 1b. Aspheric lenses have a variable curvature, but the lens power is constant at all points, resulting in equal focus of all light rays. |
Spherical vs. Aspheric
Spherical lenses have a constant curvature on their surface, much in the same way that a sphere has a constant curvature (Figure 1a). However, the power of the lens at different points is variable, resulting in relative defocus of more peripheral light rays. Due to this constant curvature, these lenses are easier to make; however, their optics are worse. A perfectly aspheric lens has a variable curvature but a constant power even at the periphery of the lens (Figure 1b). This results in the same focus of all light rays, both central and peripheral. These lenses are more difficult to make, but their optics are better.
Peripheral light rays are relatively defocused in spherical lenses, resulting in a degradation of image quality. In an aspheric lens, the peripheral light rays are focused at the same point as the central rays, resulting in a sharper, higher-quality image.
Because of their superior optics, aspheric lenses have become the standard for high-end cameras, surgical microscopes, slit lamps and even high-quality glasses and contact lenses. In fact, for nearly 50 years ophthalmologists have been using aspheric 20 D lenses to examine retinas via the binocular indirect ophthalmoscope.1 The benefits of the aspheric 20 D lens are many: the image quality is good, there is no distortion of the image at the periphery of the lens and the lens is relatively immune to decentration or tilt. For comparison, try examining the retina with the 20 D from your spectacle trial lens set.
Classification of IOLs
We can classify IOLs as either spherical or aspheric. Spherical IOLs have positive spherical aberration. The aspheric category is subdivided into lenses with zero spherical aberration and those with negative spherical aberration.
The traditional IOLs with positive spherical aberration are currently the most commonly used lenses for pseudophakia. This is likely to change, as these IOLs give a poorer quality image than the aspheric IOLs in the vast majority of patients.
The zero aberration IOL that is available in the U.S. market is the SofPort AO Advanced Optics silicone IOL (Bausch & Lomb, Rochester, N.Y.). This same aberration-free optic design will be used on the company's Akreos AO acrylic IOL, which will likely be available in the United States in the near future. This zero spherical aberration design is achieved via aspheric anterior and posterior surfaces of the IOL.
|
|
|
Figure 2. The spherical aberration of the lens and the eye as a whole increases with age, with the most dramatic change due to implantation of standard IOLs, which can induce high levels of positive spherical aberration. |
The negative spherical aberration aspheric IOLs that are available include the Tecnis line of IOLs (Advanced Medical Optics, Santa Ana, Calif.) and AcrySof IQ IOL (Alcon, Fort Worth, Texas). The Tecnis line includes silicone (model z9001) and acrylic IOLs (model z9003), both with modified prolate aspheric anterior surfaces. The AcrySof IQ lens is a single-piece yellow acrylic IOL with the posterior surface modified.
I have used each of the above aspheric IOLs in my own practice, and each has its merits. However, the IOLs with positive spherical aberration will rarely outperform the aspheric IOLs. I have removed the traditional spherical IOLs from my surgery center consignment as I feel that 99% of the time, there is no reason to implant an IOL with positive spherical aberration.
How the Eye Changes with Age
The normal human cornea has a mild amount of positive spherical aberration, which is cancelled out by the mild amount of negative spherical aberration present in the young crystalline lens.2 While the cornea's level of mild positive spherical aberration stays relatively constant throughout life, the crystalline lens changes. The young crystalline lens has negative spherical aberration, but it moves in the positive direction with age. In middle age, the lens has zero aberration and as the cataract develops it moves toward positive spherical aberration.3,4
The most dramatic change happens at the time of cataract surgery, when a traditional IOL is implanted. This dramatically increases the amount of positive spherical aberration in the eye (Figure 2). Studies have shown that for age-matched eyes, pseudophakic eyes have significantly more positive spherical aberration than the cataracts they replaced.5
By implanting an IOL with negative spherical aberration, we can aim to offset the mild amount of positive spherical aberration present in the normal cornea. This gives a total of zero spherical aberration to the eye as a whole, as was the case at 25 years of age.
By implanting an IOL with zero spherical aberration, we leave the eye with the mild amount of positive spherical aberration that is present in the normal cornea. This leaves the eye as a whole with a small amount of spherical aberration, similar to a normal 45-year-old eye.
|
|
|
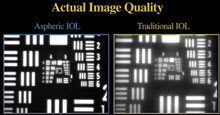
Figure 3. Comparison of image quality of a photo (left) taken through a 22 D Aspheric IOL (SofPort AO) and a 22 D traditional IOL (SofPort SE), though a camera with a 5-mm pupil size (right). |
Spherical Aberration Degrades Image Quality
We know from our experiences with corneal-based refractive surgery that there is far more to vision than Snellen acuities. Contrast sensitivity is an important determinant of the quality of vision, and the more spherical aberration that the eye has, the poorer the quality of vision is. Studies have shown an improvement in simulated driving reaction time in patients with the Tecnis aspheric IOL.6
Perhaps the best example of the difference among image qualities between spherical and aspheric lenses is obtained by taking a photograph of the U.S. Air Force test targets as seen through actual IOLs (Figure 3). When we compare the image quality of the photographs, the improvement with an aspheric IOL compared to an IOL that has spherical optics but is otherwise identical (same power, same material, same design, same manufacturer) is dramatic.
Relationship of Depth of Fieldto Image Quality
With other factors such as pupil size, ambient lighting and other aberrations kept constant, the effect of spherical aberration on depth of field is inversely related to the image quality of the eye (Figure 4). With less spherical aberration, the image quality is better, but the depth of field is decreased. Similarly, with more spherical aberration, the image quality suffers, but the depth of field is increased (Figure 5). The depth of field in this case is related to the splay of the light rays around the focal point.
In the young 25-year-old eye, the zero spherical aberration status of the eye as a whole minimally affects the depth of field due to the dynamic accommodation, which can change many times in just a fraction of a second, as can the other determinants listed above. However, with these fixed focal point monofocal IOLs, there is no longer any accommodation. There is, unfortunately, no substitute for youth.
|
|
|
Figure 4. Depth of field is inversely related to the image quality with respect to spherical aberration. |
Which IOL for Which Patient?
With three distinct classes of IOLs, which IOL do we choose for which patient? To properly match the IOL to the patient, the questions that I ask are:
■ What is the patient's mesopic or scotopic pupil size? Since the peripheral light rays are the ones that are most affected by spherical aberration, if the patient has small pupils at all times, he is unlikely to notice the difference between an aspheric IOL and a traditional IOL.
■ What are the patient's requirements for vision? Patients who are active, still working, still driving at night and are more demanding are more likely to notice the difference between aspheric and traditional IOLs.
Patients who spend a considerable amount of time at a fixed focal point, such as professional drivers watching the road, would benefit from the best possible image quality, even if it means a decreased depth of field. A half-diopter depth of field at distance can equal many yards, whereas a half-diopter depth of field at near can equal just a few inches.
■ How hyperopic is the patient? The amount of spherical aberration increases with dioptric power in traditional IOLs. Therefore, the patients who need a +28 D IOL will have significantly more induced spherical aberration than those who need a +14 D IOL.
■ Has the patient had previous corneal refractive surgery? A patient with a history of prior myopic refractive surgery likely has flattening of the cornea with a resultant increase in the corneal positive spherical aberration. In this case, implanting an IOL with negative spherical aberration will help to offset this change and will result in better visual quality.
A patient with a history of prior hyperopic refractive surgery likely has steepening of the cornea with a resultant decrease in the corneal spherical aberration, often to the point of negative spherical aberration. By implanting a traditional IOL that induces positive spherical aberration, we can help to balance out this change and give better visual quality. This is one of the rare situations where a traditional IOL will outperform an aspheric one.
|
|
|
Figure 5. When we compare the three classes of IOLs, we see that the best image quality comes with the least amount of splay at the focal point; however, this lessens the depth of field. |
■ How is the capsular support and what is the likelihood of IOL decentration?
The negative spherical aberration aspheric IOLs require very good centration with respect to the visual axis of the eye. Decentration of these IOLs results in a significant decrease in their performance and can even induce higher-order aberrations such as coma.7
In cases of loose zonules, irregular capsulorhexis creation or eyes likely to undergo significant capsule contraction, the centration of the IOL is variable. These eyes would do well with a zero aberration IOL because it is relatively immune to decentration.
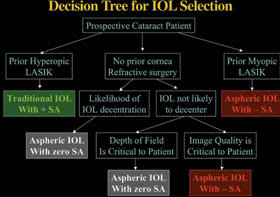
As a guideline, I have simplified my decision-making process via the simple protocol outlined in Figure 6. For the sub-selection of which negative spherical aberration aspheric IOL to use, it often comes down to yellow IOLs (Alcon AcrySof IQ) versus clear IOLs (AMO Tecnis), and that certainly is a topic for an entirely new article.
IOL Specifications
The following are detailed descriptons of the aspheric IOLs currently available in the United States.
■ Tecnis Z9001 Silicone IOL (AMO) & Tecnis Z9003 Acrylic IOL (AMO)
► The Tecnis IOLs share the same optic design and are both three-piece IOLs with 6-mm optic diameters.
►The Tecnis IOLs have about -0.27 μm of spherical aberration in order to offset the average human cornea which has about +0.27 μm of spherical aberration.
► The Tecnis IOLs perform best when they are centered within 0.5 mm of the visual axis.
■ AcrySof SN60WF IQ Acrylic IOL (Alcon)
►The AcrySof IQ is a single-piece acrylic IOL with a6-mm optic diameter. It is only available on the yellow natural platform.
► The AcrySof IQ has about -0.17 μm of spherical aberration to partially offset the average human cornea. This results in an eye with about +0.10 μm of spherical aberration for the average eye.
► The AcrySof IQ performs best when it is centered within 0.5 mm of the visual axis.
■ SofPort Li61AO Silicone IOL (B&L)
|
|
|
Figure 6. Simplified decision tree for IOL selection. Actual IOL selection depends on many factors. |
► The SofPort AO is a three-piece silicone
IOL with a
6-mm optic diameter.
► The SofPort AO has zero spherical aberration and does not add or subtract from the amount of mild positive spherical aberration present in the normal corneas.
► The SofPort AO is relatively immune to decentration and performs the same even if somewhat decentered from the visual axis.
■ AQ2015A (Staar) & CQ2015A (Staar)
► These three-piece IOLs have a 6-mm optic diameter and will be available on both the silicone and collamer platforms.
► These IOLs will be launched in late 2006/early 2007.
The Future of IOLs
IOL advances seem to come in waves. Years ago, every IOL switched to having a protective UV coating, and now it is virtually impossible to buy an IOL without it. Similarly, IOLs are now incorporating squared edges to help prevent posterior capsule opacification. The next wave is aspheric IOLs. Because of the advantages of asphericity in improving image quality with minimal downside, there will be a shift in the market toward aspheric IOLs.
It is my opinion that, within the next few years, the vast majority of all IOLs sold in the United States will be aspheric IOLs of one design or another.
Uday Devgan, M.D., F.A.C.S. is in private practice in the Los Angeles area. He is an associate surgeon at the Maloney Vision Institute and an assistant clinical professor at the Jules Stein Eye Institute at the UCLA School of Medicine. Dr. Devgan also serves as the chief of ophthalmology at Olive View – UCLA Medical Center in Sylmar, Calif. He can be reached via e-mail at devgan@ucla.edu.
References
1. Christensen RE. The use of an aspheric lens for indirect ophthalmoscopy. Am J Ophthalmol. 1959;48:256-257.
2. Wang L, Koch DD. Age-related changes in corneal and ocular higher-order aberrations. Am J Ophthalmol. 2004;135:897.
3. Glasser A, Campbell MC. Presbyopia and the optical changes in the human crystalline lens with age. Vision Res. 1998;38:209-229.
4. Artal P, Berrio E, Guirao A, Piers P. Contribution of the cornea and internal surfaces to the change of ocular aberrations with age. J Opt Soc Am A Opt Image Sci Vis. 2002;19:137-143.
5. Alio JL, Schimchak P, Negri HP, Montes-Mico R. Crystalline lens optical dysfunction through aging. Ophthalmol. 2005;112:2022-2029.
6. Packer M, Fine IH, Hoffman RS, Piers PA. Improved functional vision with a modified prolate intraocular lens. J Cataract Refract Surg. 2004;30(5):986-992.
7. Wang L, Koch DD. Effect of decentration of wavefront-corrected intraocular lenses on the higher-order aberrations of the eye. Arch Ophthalmol. 2005;123(9):1226-1230.