technology
Digital Technology Maximizes Profitability
If
you are not there yet, time is running out.
BY
RICHARD EDLOW, O.D.
|
As we begin our discussion of specific devices and software, here is a list by category, of many of the necessary items for transitioning to an electronic office: |
|
|
EPM:
• Card scanners: insurance cards |
Optical:
• Inventory scanners |
| EMR:
• Diagnostic Equip: EPIC, HVF, IOL Master, HRT, OCT |
Miscellaneous, Staff Training:
• Allergan Access |
| Marketing:
• Patient Education DVDs |
|
Timing is everything. Five years ago, our practice had automated diagnostic equipment, patient education software and patient insurance and demographic information all captured in a practice management software package. Patient prescriptions were still written manually and we had a forest worth of paper strewn about.
No one item communicated with another. Everything stood on its own, which produced unnecessary redundancies, lost or misplaced charts and significant loss of productivity.
This same scenario exists needlessly today in approximately 85% of all ophthalmic practices. Over the past 3 to 5 years, most manufacturers and vendors of practice management equipment, software, electronic medical records (EMR) systems and diagnostic testing equipment have made great strides in tying all of the components together. Practices can no longer ignore this dramatic convergence of technology if they wish to remain competitive.
Take a close look at just about any industry and the challenges are similar. There are always market forces that help to drive or force innovation. These include price competition, new technology, productivity demands, human resources and financial management. The healthcare industry in general, and the eyecare segment in particular, has certainly experienced many of these forces, yet has been slow to adapt. In this article, I will review the market forces and present a solution, based upon embracing all available technology, to maximize practice productivity and profitability.
Price Competition
Price competition comes primarily from three sources in eye care. First, many studies have shown that there is a relative oversupply of eyecare providers (both ophthalmologists and optometrists). With the way eyecare providers are geographically distributed throughout the country, one might agree that it is difficult to increase prices for goods and services. This is borne out by the Bureau of Labor Statistics Eye Care Index (a component of the Consumer Price Index, CPI) which has remained not just on pace with the CPI, but which actually shows a deflationary trend since its inception in 1986. From 1986 to 2006, the CPI increased 79.9%, the Medical Care Index increased 179.2%, yet the Eye Care Index increased only 63.2%. This certainly supports the oversupply theory in economic terms.
|
|
|
Figure 1. A card scanner from New Soft Inc. |
Additional outside constraints on price competition come from government decree, as in Medicare and Medicaid payment strategies that we, as practitioners, have little control over and third-party private payers who consistently attempt to negotiate volume discounting which further encourages productivity improvements.
New Technology in Eye Care
New technology abounds in eye care. Simply look
around at all the new diagnostic procedures that dramatically improve our clinical
management and enhance patient care. Just about every new piece of equipment has
an output that is electronic and digital for potential interfacing with other equipment.
Technology can have
significant impact on every aspect of the practice, from
patient check-in and registration to patient work-up and education, medical records
documentation and billing and collections.
Increased Need for Eyecare Services
Productivity demands are going to be a major force in eye care for the next 20 years. As we know from daily experience, an individual's need for eyecare services increases almost exponentially from 40 years of age. The prevalence of age-related eye disorders is anticipated to increase 50% from 2000 to 2020 (Archives of Ophthalmology, April 2004). From 2004 to 2014, the number of Americans between 55 and 64 years of age will increase by over 10 million (U.S. Census Bureau).
|
|
|
Figure 2. A Galvanon Medical Kiosk for patient check-in. |
It might be easy to ignore these statistics as the recent past failed to produce the huge increase in cataract procedures, and age-related eye care in general, that so many predicted. The reason for the miscalculation is simple; we were coming off the post-World War II/pre-baby boomer period whereby those 65 years of age and older were a relatively flat percentage of the U.S. population. This is about to dramatically change within the next 4 years, which should give us enough time to prepare.
Someone born in 1945 (the last year prior to the baby boom) will not turn 65 until 2010. The prevalence of cataracts, as an example of age-related eye disorders, is just 16% for those 45 to 64 years of age, 31% for 65 to 75 years of age and 49% for those 75 years of age or older.
Productivity Demands
Productivity demands will be a major a factor as we plan for our practice's throughput capability and physical structure needs for the near future. If we simply consider a growth rate in patient encounters of 10% per year, in just 7 years, patient volume will double. This article will demonstrate how we have been able to prepare for this growth by continually embracing the confluence of all the available new technologies.
Employment data imply that in the United States, we are essentially at full employment and the challenge of locating skilled and enthusiastic staff members for our practices is overwhelming. Here again, application of various new technologies dramatically shortens the learning curve for new staff. Electronic medical records (EMR) and associated/interfaced technology can have a significant and positive impact on both the practice and quality of patient care.
Benefits of Technology
|
|
|
Figure 3. A signature pad from Interlink Electronics. |
Patient care, practice management, productivity gains and staff education are not the only benefits of today's technology convergence; financial and cash management are other benefits. Combining electronic practice management (EPM) with EMR will produce better cash flow and reduce days-out accounts receivables. Claims will be turned around more quickly and denials handled "on-the-fly."
While the focus of this article is primarily on the interfacing of technology on the clinical side of the practice, we must not ignore all that is available on the business or practice management side. Here is a brief review of what is available:
■ Card scanners that interface with EPM simultaneously scan both sides of the patients' insurance cards and imbed the images in the patient record (Figure 1). Waiting room computer kiosk stations allow patients to confirm their demographic information and also pre-enter their medical history and medications (Figure 2). Digital cameras can record the patient's photo for future reference and easy recognition.
■ Electronic signature pads allow capture of the patient's signature for acknowledgement of HIPAA privacy statements as well as insurance assignment and financial responsibility (Figure 3).
■ Electronic claims submission and electronic remittance of payments allows hours spent sending out insurance claims and posting explanation of benefits work to be processed and completed in a matter of minutes.
|
|
|
Figure 4. An EPIC refraction system from MARCO. |
■ Patient statements and recall notices can be electronically generated processed and delivered by an outside third party with the click of a mouse.
■ Database mining software has recently been developed to assist in recapturing patients who have failed to respond to recall notices and would normally be lost to follow-up. In addition, telephone confirmation calls are now performed electronically with a human voice via access to the scheduling database, saving your staff time.
Adoption of these practice management techniques can allow for significant practice growth without adding human resources or physical space.
Using EMR Technology During an Exam
It is on the clinical side with EMR that technological advancement really shines. Let's run through what might be a typical comprehensive eye exam. Once the patient has been electronically checked in by the receptionist, the clinic manager's computer monitor will indicate that the appointment has been kept, what type of exam and testing the patient is scheduled for and for which doctor. While this is occurring, the patient is in the front waiting room probably viewing a 42-inch flat-panel monitor explaining the latest multifocal lens implants or a newly developed progressive lens.
|
|
|
Figure 5. A Chart Note with visual field in EMR on monitor. |
The clinic manager might preview the patient's chart, which is never missing, and then assign a technician to bring the patient back to a pre-testing room where the patient's lensometry, keratometry, objective refraction, wavefront analysis and subjective refraction are all performed in a matter of 6 to 8 minutes.
All of this data is immediately uploaded and captured in the patient's EMR chart without ever picking up a pen or piece of paper. This translates to no transcription errors and a savings of about 2 minutes per patient (Figure 4). Note: please multiply 2 minutes by the number of patients seen per day to realize the advantages to EMR.
The doctor may have ordered a visual field or nerve fiber analysis which is then performed and again, electronically captured into EMR (depending on equipment, this capture might be a direct-map interface or simply a scan into the patient's EMR [Figure 5]).
The patient then enters the exam room. The ophthalmic technician records the patient's chief complaint and updated medical and ocular histories with several clicks of the mouse (selecting the appropriate responses from drop-down pick lists) or keyboard entry for more unusual responses. This results in a legible, readable, correctly spelled comprehensive history, all of which is continually calculated to help arrive at the appropriate level of coding for the current visit.
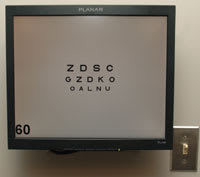
Visual acuity is precisely measured and recorded from the constant level illumination (no more projector bulbs to burn out) of the liquid crystal display (LCD) monitor displaying letters that have not been memorized (random changing of letters, perfect for those patients requiring multiple follow-up visits [Figure 6]). Since with EMR a computer CPU box already sits under the counter in the exam room, LCD acuity monitors are not only affordable but clinically superior. All that is needed is a modestly priced 17-inch monitor with a wall mount, video cable, dual-video card for the computer and the proper visual acuity software, such as the Provideo acuity system (Innova Systems, Burr Ridge, Ill.) which includes the wireless remote.
|
|
|
Figure 6. An Innova Provideo acuity system running off EMR computer CPU. |
As the exam continues, entries are made with a series of mouse clicks and an occasional keyboard stroke. Visual acuities, IOPs, and C/D ratios can all be instantly viewed over time with imbedded serial tables. If an anterior segment or fundus photo is required, it is digitally captured and conveniently resides in the patient's EMR. With a click of the mouse, one can instantly view the patient's previous visual fields and nerve fiber analysis, consult reports, ultrasound or topography results.
Our sample patient might need to be dilated. While waiting for dilation, a patient-education software loop can be played on the exam room computer related to the patient's condition or upcoming optical needs (Figure 7).
As the exam comes to an end, the doctor or scribe clicks the appropriate diagnoses (which automatically sends it over to EPM to match up with the proper CPT code for billing), which in turn prompts the appropriate treatment plan(s). Pharmaceutical prescriptions are created and legibly printed or electronically faxed directly to the patient's pharmacy. Optical prescriptions are printed or sent to the in-house optical dispensary.
We are alerted to all the additional testing performed throughout the patient's visit and prompted to bill for these, when appropriate. Also at this point, we select the appropriate level of CPT code, which has been calculated throughout the exam, as each component of the exam is recorded.
The
next step is a prompt for a report to be generated for the patient's primary care
physician, if the patient is diabetic, and a report goes to the referring doctor.
With a single mouse click each of these are instantly produced. Finally, a complete
chart note is generated covering the entire exam. This is done without dictation
and without transcription services, before the patient even gets up from his chair.
Figure
7. An EyeMaginations video loop for patient viewing.

Billing information is completed before the patient makes his way up to check-out. Patient education forms are customized and printed (for example, how to perform lid scrubs or pre-operative instructions). If surgery is being scheduled, the proper consent forms are printed out with the patient's name, date of birth and operative eye. The possibilities are limitless.
Benefits of Interfacing EPM and EMR
The interfacing of EPM and EMR functions produces additional opportunities throughout the ophthalmic practice including the optical dispensary, staff training and direct-to-patient marketing.
Over the years, the traditional approach with an optical dispensary is for the patient to present the optician with a written optical prescription and then give the optical staff insurance information as well as basic demographic data. All of this redundancy is eliminated. With properly interfaced optical EPM and EMR software, the patient simply presents to the optical dispensary and the staff already has the patient's basic demographic and insurance information in the system. The final spectacle and/or contact lens prescription is simply imported with the click of the mouse.
Patients are aided in their appreciation of lens treatments and features by viewing the applicable video clips presented on the dispensing table's flat-panel monitor. New contact lens patients are able to reduce their insertion and removal (I&R) training time by over 50% by simply viewing the animated I&R training clip. For at-home viewing, the patient is advised to view the I&R information by clicking a link on the practice's Web site.
Frame, lens and contact lens inventory is now readily tracked, entered and removed with the swipe of the bar code reader (Figure 8). Billing information is now built-in, in much the same manner as the CPT and ICD-9 coding found in the EMR system. The major national labs interface with the optical dispensary for ordering and job tracking.
|
|
|
Figure 8. A bar code scanner for frame and lens inventory. |
Hiring Staff with No Previous Experience
With the difficulty of attracting experienced ophthalmic tech staff, today's practices find themselves hiring individuals who have zero previous experience. The length of the training cycle can be dramatically shortened by taking full advantage of these new technologies. New staff members can be given a period of time to view all of the patient education software that resides in every exam room. They can be required to satisfactorily complete every training module available via the Allergan Access Web site (Our office requires every new staff member to not only complete each module, but also score 100% on every end-of-module exam). Other vendors have initiated on line training for their diagnostic equipment (for example, Marco Technologies' EPIC refractions).
Probably the most dramatic training catalyst is EMR; the logic and standardization built into the EMR system takes what was previously a paper medical record with infinite variables, and transforms it into a consistent pattern and flow on the computer.
Richard C Edlow, O.D., is chief operating officer of the Katzen Eye Group, a leading eye care practice in the Baltimore area. Katzen Eye Group has implemented a technologically advanced electronic medical records system. Dr. Edlow is chair of the Information and Data Committee of the AOA. Dr. Edlow would like to acknowledge the assistance of Janna Mullaney, Practice Administrator, in development of this article. He may be reached at www.katzeneye.com