practice
Building an Elective Vision Practice
Overcoming the four barriers to success.
BY KAY COULSON
The ophthalmology landscape changed in May 2005 when the Centers for Medicare and Medicaid Services (CMS) allowed ophthalmology practices to offer and charge for presbyopia-correcting lens implants. Over the past 15 years, practices have evolved as either refractive or comprehensive, but for the most part, this really meant elective private-pay services or insurance-billed services. Now that IOLs and phakic lenses have moved into the elective domain, many practices are confused about how to introduce new private-pay services to their traditional patient bases.
In this article, I'll explain how to build a successful elective vision practice by eliminating the four key barriers that can limit or prevent success.
New Opportunities
The traditional "refractive center" model is focused on LASIK. How should it add an elective lens service line into the mix? This different patient – often older –might not fit with the LASIK image the practice has cultivated. Surgeons and facilities need to be credentialed by insurance panels, as most lens patients have cataracts and expect the benefit of partial insurance coverage.
The traditional "comprehensive ophthalmology" practice model is built around insurance assignment and maximum patient throughput. Packed appointment schedules, long patient-wait times, diverse pathology and treatment requirements, and surgeons confounded by the thought of introducing even one more activity into their day, characterize a typical comprehensive mindset.
What I have learned in working successfully with various refractive and comprehensive ophthalmology practices is that there are key reasons why practices fail to build vibrant, viable, elective vision service lines. Many surgeons and administrators say, "My practice is different" or "My patients are different." I respectfully refute this notion. The problems I have seen, and the patients I have counseled and interviewed, confirm commonality rather than dissimilarity. Using the "We're different" excuse really means, "We won't change." But that would be a serious practice-limiting mistake. Ophthalmology is leading the way in elective medical services. No medical specialty has done a better job of educating, performing and collecting fees for permanent vision care than ophthalmologists through LASIK. We now have a huge new market open to elective vision choice with presbyopia-correcting lenses. Elective vision now covers corneal and anterior segment surgery. Indeed, the defining distinction of elective surgery is really "permanent" vision. What can we do at various life stages to allow people to be glasses-free? Practices that understand the power of "glasses-free" — through LASIK, conductive keratoplasty (CK), phakic lenses, presbyopic IOLs and all the technologies yet to come — will prosper in the elective vision world.
Overcoming the Obstacles
Four barriers prevent elective vision success: poorly defined practice goals; an unstructured, undisciplined appointment calendar; low surgical conversions and a poor grasp of financial leverage within a practice. Eliminate these barriers and you are on a path to creating a successful elective vision practice.
Poorly Defined Goals
When I begin an engagement with a new practice, I ask the participating surgeons three things.
► What types of patients do you want
to see?
► How much do you want to work?
► How much do you want to earn?
Having a competent administrator is key in building your appointment calendar and practice income statement to deliver these goals. How is your appointment calendar currently scheduled? Most likely, the old-fashioned way — first-in, first-out with whomever calls. Somewhere between day 1 when a physician hangs out his shingle, anxiously scheduling and accommodating each patient for fear of turning business away, and day 5,000 — when the practice is overrun with red eyes, pressure checks, visual fields and surgery — the notion of building a focused surgical practice is lost. Now is your time to reclaim that vision. Define the types of patient(s) you want to see and build a calendar to support this goal.

The most common appointment calendar errors I see are too little definition/segmentation in the appointment types, too little structure in creating scheduling blocks and repeated scheduling violations by untrained or undisciplined staff.
Appointments should be defined by type: consults/evaluations, exams, rechecks, surgery and post-ops. You must identify the feeder visits that fuel your practice. If you want to do more surgery, your appointment fuel must be exams and consults. If you have an appointment calendar that provides no more detail than "short visit" or "long visit," you have no idea if your fuel level is appropriate.
Once you have decided how many of each visit you need to see weekly to deliver surgical goals, develop a scheduling template that allows your staff to succeed. Where in your medical oath to "Do No Harm" was it written that you must see all types of medical conditions all days of the week? Give yourself time to think and educate and succeed by creating LASIK consult days, lens evaluation days and glaucoma/pathology days. Many of you will say, "But I must give my patients a choice. They won't all come on Wednesdays." The reality is, you currently don't give them a choice. Your appointment scheduler says, "We have this date/time available." I see practices that take pleasure in saying, "We're booked 3 months out." Any practice that cannot see their key visits within 2 weeks is sending revenue to the elective practice down the street. You are clogged with non-critical, staff-draining, revenue-bleeding visits that will not grow your surgical practice. Creating dedicated appointment days gives like-minded patients a time completely focused on their needs. These blocks improve your timeliness, your profitability, your bedside manner and your patients' satisfaction with your practice.
Finally, you must stop wayward staff members from sabotaging the schedule. I often view appointment calendars that label 30% of daily visits as work-ins or fill-ins. This is outrageous. Are these emergencies? Pressure checks? A consult that asked to be seen today? How can your scheduling template have so little structure that you cannot track what you see patients for? Why do you allow schedulers to book and double-book patients, expecting that technicians will sort it out on the day of the appointment? These violations will not sort out. Instead, 25 people will be sitting in your waiting area, each more frustrated than the next that you cannot run your practice efficiently.
What is the solution? Define your surgical goals. Determine, based on demonstrated conversion, how many consults/evals you need to see in a week to deliver this goal. Create a template that allows you to schedule, measure and track your success in seeing these patients.
Poor
Conversions
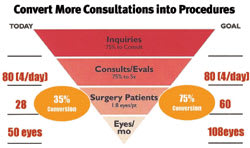
Conversions are the primary driver in a LASIK practice, and will become the primary driver in an elective lens practice. Successful practices have moved from generating more calls to converting each call that comes in more effectively. Ideally, an elective practice should convert 75% of inquiries to consult and 75% of consults to surgery. This means one out of two people move on to surgery. In reality, many practices convert far less.
When I ask a lens surgeon how many people he or she has seen in the last month who were diagnosed with a cataract and scheduled to surgery, the answer is always 90% to 95%. However, when I perform the math, the story is quite different. An insurance-based cataract surgeon performing 50 surgeries per month tells me he sees 40 patients per day on average. Review of his appointment calendar confirms the 40 daily appointments and indicates that 10 of these patients each day are potential lens surgeries — either cataract evaluations referred in from optometrists, cataract rechecks from within his own practice or people over the age of 50 who present for an annual exam with symptoms of glare consistent with a cataract. Ten patients per day equals 40 per week (assuming 4 clinic days per week.) That potential is 80 lens surgeries per week, or 360 per month. Yet the surgeon is performing 50. Rather than 90% conversion, my experience is that general ophthalmology practices convert no more than 20% of patients to surgery. Patients may tell the surgeon they will schedule, but then back out with the surgery scheduler, cancel after returning home, don't pass medical clearance or opt-out because they don't have the funds.
If you believe your surgical conversion rate is 75% or higher, apply a bit of critical reasoning to your own appointment calendar. How many cataract evals, cataract rechecks and annual exams do you see on average per week. Does this number match with what is ending up on your surgery schedule? How much surgery exists (elective or insurance-based) that has not moved forward? How can you improve the scheduling and retention of these patients? What is happening within your practice that causes patients to delay or cancel surgery? Why do you keep these patients in a perpetual recheck cycle until they are 85 with rock-hard cataracts, when you can offer them monofocal or multifocal lens surgery today that improves their daily life?
Poor Grasp of the Financials
If you accept that moving all of your lens exams to a single day will improve your surgical conversion, try this. Book patients every half hour with the visit lasting 1 hour, comfortably scheduling 15 patients on this day.
When I suggest this idea, I immediately hear from surgeons and administrators that this is impossible. There is no way they can consolidate all lens consults onto 1 day. (Conversely, the most successful LASIK practices routinely block and group their LASIK consults so they are not interrupted with dissimilar patients.) The prevailing general ophthalmology view is that 15 patients can never make up for the 50 they usually see. I hear, "This will financially cripple us." This thinking demonstrates a poor grasp of the financial leverage of appointment targeting within a practice.
On average, a comprehensive ophthalmology practice that sees 50 patients per day ultimately collects $5,000 per day, or $100 per visit. This averages reimbursements from refractions, to exams, to testing, to surgery. By concentrating on 15 lens consultations in a single day, a potential 30 surgical eyes, 80% of patients will schedule surgery that day (compared to the meager 20% that actually schedule now). Seventy-five percent will chose a monofocal insurance lens, and 25% will choose an upgraded presbyopic lens, because you have taken the time to counsel and educate them on the benefits of full-range vision. These 15 patients yield $16,000 in physician surgical fees, not counting increased facility fees that result from higher conversions. One-third the patients — three times the revenue. The bottom line is happier, on-time, educated patients excited about their vision-improvement options. The practice, the surgeon and the patient all benefit in this scenario.
Better Focus Brings Rewards
Improving your ophthalmology practice does not mean running faster on the wheel. It does mean choosing the type of practice you want and building a schedule that rewards your focus. If you desire increased surgical volume, and a vibrant elective vision practice, examine these barriers to see what is holding your practice back from optimal performance. Your patients' satisfaction — and your quality of life — depend on it.
Kay Coulson is founder of Elective Medical Marketing and Course Director for the Alcon-sponsored Revolutions in Laser and Lens Surgery Practice Development program. She helps surgeons build their elective vision service lines. She can be reached at kay@electivemed.com








