imaging
Anterior
Segment Imaging with the Visante OCT
BY
ELLA G. FAKTOROVICH, M.D.
|
|
|
The Visante OCT from Carl Zeiss Meditec. |
In recent years, optical coherence tomography (OCT) has been used with increasing frequency to visualize and measure the posterior pole. Now we have the same advanced diagnostic capabilities for the anterior segment with the Visante OCT (Carl Zeiss Meditec, Inc., Dublin, Calif.). Detailed pachymetry maps, high-resolution corneal images and precise anterior-chamber depth calculations increase precision accuracy in diagnosis and follow-up of patients with corneal thinning disorders, narrow angles and those presenting for refractive surgery. Just as with the posterior segment, the OCT is now an invaluable tool for advanced anterior segment diagnostics.
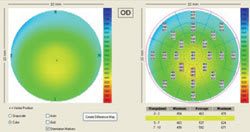
A Detailed OCT Pachymetry Map
When checking corneal thickness, probe placement and repeatability can be an issue when detecting or following keratoconus. If a patient's corneal thickness shows a decrease a year later, is it because the probe was placed in a different spot or is there true thinning?
|
|
|
Figure 1. A normal pachymetry map with gradual and symmetric corneal thickening toward periphery. |
The Visante OCT maps corneal thickness in 25 spots across the cornea and has great repeatability (Figure 1). It can also create a differential map to compare past readings and detect subtle changes involved in corneal-thinning conditions. This can be very useful in following a patient with keratoconus or pellucid marginal degeneration (Figures 2a-b).
The OCT is an effective tool in refractive surgery screening. Even if the corneal topography is symmetric and central-ultrasound pachymetry is normal, the OCT pachymetry map can reveal an abnormal pattern of corneal thickness, raising suspicion for forme fruste keratoconus (Figure 3a-b). The other eye of this patient does, in fact, have clinical keratoconus.
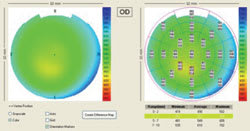
The OCT pachymetry map is especially useful in screening patients with thinner corneas by ultrasound pachymetry. Even if their topography is symmetric, the OCT can reveal an asymmetric pattern of corneal thinning. Consider a patient with a symmetric topographic map and central ultrasound pachymetry of 490 μm (Figure 4a). Looking at this patient you may think that PRK is a possibility, but more information about the overall corneal thickness pattern, especially inferior vs. superior cornea, would be helpful. The OCT pachymetry map (Figure 4b) reveals inferior thinning that may sway you not to perform any corneal refractive surgery on the patient.
|
|
|
|
Figure 2a (top). Corneal topography of a patient with pellucid
marginal degeneration. |
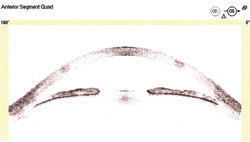
High-Resolution OCT Corneal Scan
Postoperatively, high-resolution corneal scans detail the actual thickness of the flap and the residual stroma. This is useful in ensuring that enough residual stroma will remain after an enhancement. For instance, the patient in Figure 5 had LASIK 6 years prior to presenting to us with -2 D. Her medical file was unattainable so there was no preoperative or intraoperative information available to us.
We could perform the ultrasound pachymetry, but there would be no differentiating between the flap and the stromal bed thickness. Alternatively, we could take this patient into the operating room, lift the flap and perform the ultrasound pachymetry on the stromal bed, and if there was enough stromal bed, we could then perform the excimer enhancement.
The patient in Figure 6 had LASIK performed 4 years ago and presented to us for a possible enhancement of -5 D. In her case, there was too little stroma left (255 μm) and she could have been put at risk for ectasia if we performed an enhancement. Another option would be to perform PRK. By measuring the thickness of the epithelium and the thickness of the flap, we could see if there was enough stroma within the flap to treat the residual refractive error without creating a buttonhole.
High corneal resolution scans can also be used to measure the depth of conductive keratoplasty spots and evaluate the pattern of collagen shrinkage in each spot (Figure 7).
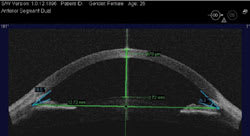
OCT Angle Depth Calculation
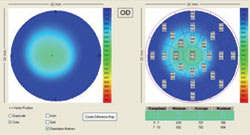
With OCT, we can visualize the anterior chamber in great detail. This is useful in evaluating glaucoma suspects (Figures 8, 9 and 10). Angle depth measurements are subjective and can vary from exam to exam. Using the slit lamp to grade the Van Herrick angle is a good gauge, but prone to observer bias. Gonioscopy, although necessary to directly visualize the angle, may introduce not only observer bias, but compression bias as well. The subjectivity and dependence on the technique of these tests may cause narrow angles to be under-diagnosed.
|
|
|
|
Figure 3a (top). Corneal topography (left) showing flat, but symmetric corneas. Central ultrasound pachymetry is 600 μm. Figure 3b (bottom). The OCT pachymetry map (below) reveals a localized area of corneal thinning, raising suspicion for forme fruste keratoconus. |
With the OCT scan, the user can visualize the angle in multiple cross-sections of the anterior chamber. Because the OCT uses infrared light, the pupil does not constrict, providing a more natural view of the angle without changing its anatomy. A measuring tool can then be used to calculate a definitive angle depth in degrees. Now, patients at risk for angle-closure glaucoma may be monitored more closely as the crystalline lens matures. Additionally, bowing of the iris can be visualized to better predict the efficacy of the peripheral iridotomy. An image of the angle may also make you feel more at ease about dilating a patient whose angles may appear borderline narrow on slit lamp exam and gonioscopy. The scan is detailed enough to even visualize Schlemm's canal and its patency or evaluate trabeculectomies.
Visante can measure every aspect of the anterior chamber accurately. Prior to placement of the IOL, it is possible to view and evaluate the chamber depth, diameter and the sulcus. This can aid in work-up of surgical candidates and help with a proper lens selection.
These are just a few of the many applications for the new anterior segment OCT. Whether it is screening candidates for refractive surgery, measuring flap thickness or calculating angle depth, the OCT is a versatile supplement to our everyday slit lamp examination.
Ella G. Faktorovich, M.D., is the director of corneal and refractive surgery at Pacific Vision Institute in San Francisco. She may be reached by phone at (415) 922-9500 or by e-mail at ella@pacificvision.org. The author has no financial interest in any of the products mentioned in this article.
|
|

|

|
|
||
|
Figure 4a
(top). Corneal topography showing symmetric cornea in a patient wearing glasses
only. Central ultrasound pachymetry is 490 μm. Figure 4b (bottom). The OCT pachymetry map reveals asymmetric inferior corneal thinning. The inferior cornea is 70 μm thinner than the superior, which could be consistent with forme fruste keratoconus. |
Figure 5. High-resolution corneal OCT scan in a patient 6 years after LASIK who presented for possible enhancement of -2 D. Flap thickness is 148 μm and the stromal bed is 351 μm — enough for the enhancement. | Figure 6. High-resolution corneal OCT scan in a patient 4 years after LASIK. The patient presented for possible enhancement of -5 D residual myopia. The residual stroma is too thin (255 μm) for further LASIK enhancements. |
|

|
| Figure 7. A high corneal resolution scan can also be used to measure the depth of CK spots and evaluate the pattern of collagen shrinkage in each spot. |
|

|
|
| Figures 8, 9 and 10. Angle depth calculation in a patient with 4+ angle at the slit lamp (Top), 2+ to 3+ angle (Middle) and a narrow 1+ angle (Bottom). Precise OCT measurement of the angle in multiple locations quantifies angle depth and eliminates the inter-observer variability allowing for accurate follow up. |