Achieving Best Corrected Vision For Corneal Transplant
Patients
Contact lenses are often the answer for these
patients. These guidelines will help you build your fitting skills.
After corneal transplantation, patients often have vision problems that spectacles cannot adequately address. The transplanted eye and the fellow eye may have significant refractive differences, such as myopia, hyperopia or astigmatism.
When these patients wear prescribed
spectacles, they typically complain of fatigue and eye strain, headaches or even double vision.
Following Prentice's rule, spectacles with significantly different corrections can cause induced
prism, leading to diplopia when patients look off the lenses' optical centers. What's more, patients
with corneal transplants also may have significant irregular astigmatism, which can't be corrected
adequately with spectacles.
Consequently, contact lenses often are the best solution for visual rehabilitation after corneal transplantation. In fact, in a 4-year retrospective study of 35 eyes fitted with contact lenses for visual rehabilitation after penetrating keratoplasty, 70% had improved Snellen visual acuity versus that achieved with spectacle correction.1 Mean best-corrected visual acuity was 20/30 with contact lenses, compared with 20/40 with spectacles alone. More importantly, binocular function was greatly improved in patients using contact lenses vs. spectacle correction, when there was significant spherical or astigmatic anisometropia.
|
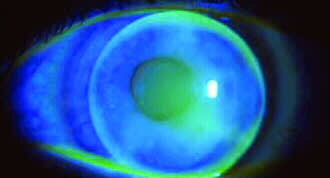
Fluorescein
photo of a corneal transplant showing proper |
Fitting contact lenses after corneal transplantation can be challenging, but it's an essential element of visual rehabilitation for these patients. Here are some guidelines to assist you.
Goals and Challenges
Not only is there a physiological difference
between the transplanted cornea and that of the fellow eye, but the transplantation surgery itself
also can produce problems with visual acuity, including
irregular astigmatism and significant spherical or
astigmatic anisometropia.
In addition to achieving the best vision correction, you must be mindful of the fit. If the contact lens is not properly aligned with the transplanted cornea, problems such as corneal chafing may develop. For a well-centered lens and to avoid chafing or having the edge of the contact lens ride on the graft-host margin, you need to choose an appropriate posterior base curve, as well as a lens that completely covers the corneal transplant. By slightly vaulting the lens over the graft, as shown in the photo above, you can significantly control corneal chafing.
Choosing the Lenses
Generally, you'll achieve the best results
by fitting post-corneal transplant patients with high-Dk spherical gas permeable (GP) lenses.
I prefer this material for several reasons:
1. Compared to standard hydrogels,
GP lenses deliver more oxygen to the cornea, a critical need of the transplanted cornea.
2. There is a very low incidence
of infection associated with GP lenses.
3. These lenses hold their form,
negating corneal astigmatism better than toric soft contact lenses do.
4. They maintain a more regular
refractive surface, resulting in better visual acuity.
For difficult-to-fit high astigmatism
cases, bitoric GP lenses may be helpful. Their two posterior curvatures, located 90 degrees apart,
can better contour to the ocular surface.
In some cornea transplant eyes,
the graft is flatter than the peripheral host corneal tissue. Reverse geometry GP lenses, which
are flatter in the center than in the periphery, are very helpful for these cases.
Other graft patients may benefit from a back aspheric lens design, which rides up under the upper lid and may center better. Lenticular carriers, which can be used with GP lenses, also can improve centration.
Although my first choice is usually a GP lens,
other types of contact lenses may be appropriate for specific applications. For patients with
myopic or hyperopic anisometropia, but without astigmatism, you may consider a spherical silicone
hydrogel lens, another option in the hyper-oxygen lens category.
Standard hydrogel lenses do have a very broad range of fitting parameters, and in some rare cases, such as grafts with steep curvatures, these lenses may offer better centration. However, their oxygen delivery generally isn't adequate to ensure the health of the transplant.
Potential Complications
Part of the decision-making process for fitting
contact lenses after corneal transplant is deciding not just if, but also when to fit a patient.
You need to examine the sutures to make sure they're well epithelialized and the wound margin is
stable. If you're concerned that the contact lens will chafe the wound margin, it's best to wait
for greater healing. If the eye looks ready, remove any sutures that you can to eliminate astigmatism
before proceeding to contact lens fitting.
After the fitting, watch for problems, such as corneal chafing, suture breakage, discomfort, graft thickening and infection. Allergic issues may arise, including giant papillary conjunctivitis.
Intolerance related to ocular dryness is a common but treatable condition for all contact lens wearers, but it's especially prevalent among corneal transplant patients. Neurotrophic keratitis after corneal transplantation increases dryness by de-enervating the cornea. The eye doesn't feel the need to lubricate, so reflex tearing decreases, which can cause staining. Overall, if there are no signs of corneal chafing, suture problems, graft thickening or superficial punctate keratitis, and the graft remains healthy, contact lenses are well accepted.
Gaining Experience
This is one of the most demanding contact lens
fittings we do. The lenses need to be fit as close to perfectly as possible to avoid complications.
I recommend that new ophthalmologists take every opportunity to increase their experience
and training with contact lens fitting before they take on post-transplant fittings.
Once you've mastered the skills
you need, you'll find that this is one of the most stimulating and rewarding contact lens fittings
you can do in your practice. QnMD
REFERENCE
1. Wietharn BE, Driebe WT Jr. Fitting contact lenses for visual rehabilitation after penetrating keratoplasty. Eye Contact Lens. 2004.Jan;30:31-33.
William T. Driebe Jr., M.D., is a professor of cornea/external disease and contact lens at the University of Florida College of Medicine Department of Ophthalmology in Gainesville.








