feature
The Role of Vitrectomy
in Anterior Segment Surgery
Utilizing the appropriate technique can minimize
a challenging situation.
BY
MARK PACKER, M.D., F.A.C.S., ROSA BRAGA-MELE, M.D., I. HOWARD
FINE, M.D., RICHARD S. HOFFMAN, M.D.
Vitrectomy is a word the anterior segment surgeon really does not want to say or hear. It conjures images of capsule rupture, falling lens fragments, anterior chamber IOLs, surgically induced astigmatism, cystoid macular edema and retinal detachment. When faced with the prospect of anterior vitrectomy, the immediate response of the phaco surgeon is a rapid evolution through the five stages of grief: denial, anger, bargaining, depression, and finally, acceptance.
However, surgeons can be taught to do better — we include ourselves in that number. There are definite indications for vitrectomy, and proper performance can rescue surgical results. Advances in techniques and technology mean vitrectomy no longer has to be a dirty word, or a daunting procedure.
|
|
| Figure 1. With posterior capsule rupture, the haptics of the IOL are placed anterior to the capsule in the ciliary sulcus and the optic has been tucked back behind the capsulorrhexis. |
Separation of Irrigation and Aspiration
The first time most surgeons experienced the separation of infusion from aspiration in the anterior chamber is during the performance of anterior vitrectomy in cases of unplanned vitreous loss. Today, we can utilize an irrigating chopper or manipulator in one hand and a phaco needle in the other hand while performing all cataract and lens extraction procedures with bimanual microincision phacoemulsification.1
Lens extraction performed through two paracentesis-type incisions offers unique advantages that enhance surgical control and safety. The crucial difference is not the size of the incisions; it is the separation of inflow and outflow. This same separation of inflow and outflow facilitates the performance of anterior vitrectomy, for many of the same reasons.
Separation of irrigation from aspiration allows for improved followability by avoiding competing currents at the tip of the phacoemulsification needle or automated vitrector. In some instances, the irrigation flow from the second hand piece can be used as an adjunctive surgical device — flushing nuclear pieces from the angle or loosening epinuclear or cortical material from the capsular bag. In refractive lens exchange, the lens material may be washed completely out of the bag and extracted with aspiration and vacuum only, so that no ultrasound is used and no instrument enters the endocapsular space, increasing the safety profile of this demanding procedure. The flow of fluid from the open end of an irrigator represents a very gentle instrument which can mobilize material without trauma to delicate intraocular structures.
Another benefit of a separate infusion stream comes to bear in polishing the posterior capsule. Focusing the flow of fluid on the posterior capsule and putting the tissue on stretch facilitates capsule polishing with either a roughened or silicone-covered aspiration tip. The taut posterior capsule shows less inclination to become entrapped in the aspiration port, and the subcapsular plaque material is more easily stripped away.
Bimanual Benefits
Perhaps the greatest advantage of the bimanual technique lies in its ability to remove subincisional cortex without difficulty. As originally described by Brauweiler, by switching infusion and aspiration hand pieces between two symmetric incisions, 360° of the capsular fornices are easily reached and cortical clean-up can be performed quickly and safely.2 The ability to switch hands also represents a significant advantage to instructors of phacoemulsification, who may find they must take over a case from a resident using their opposite hands in the process.3
Bimanual phaco also provides significant advantages in complication management. If the posterior capsule is compromised during surgery, the first goal of the surgeon is to maintain stability of the anterior chamber to prevent both posterior migration of lens material and anterior prolapse of the vitreous.
By maintaining infusion in the anterior chamber, it becomes safer to use the phaco needle, aspiration tip or vitrector to remove residual lens tissue. Irrigation need never be brought down into the capsule or vitreous space, where it may dislodge lens tissue, enlarge the capsular tear or engage the vitreous.
Hypotony is avoided at all times by keeping the flow of irrigation constant, much in the same way that an anterior chamber maintainer works.4 Once all lens material has been evacuated from the eye, viscoelastic may be injected prior to removal of the irrigator so that the vitreous face remains under tamponade.
Pars Plana Vitrectomy
|
|
|
Figure 2. A slight peaking of the pupil is observed as a fluoroscein strip is applied to test the integrity of the incision. This effect alerted the surgeon to the possibility of vitreous strands incarcerated in the wound. |
In situations where nuclear remnants do fall through a rent in the posterior capsule (but remain within view), or vitreous prolapses to the wound, then the phaco surgeon should consider pars plana vitrectomy. The advantage of this approach over vitrectomy through a corneal incision resides in the fact that the vitreous gel is pulled in a posterior direction by the vacuum, thus limiting vitreous loss, preventing incarceration of vitreous strands in the incision, and facilitating a thorough clean-up of the anterior segment.
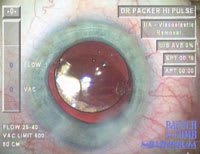
To perform a pars plana vitrectomy with 25-gauge instrumentation, irrigation is maintained in the anterior chamber with reduced pressure (lowered bottle height) as a stab incision is made with an MVR blade or other suitable instrument 4 mm posterior to the limbus, usually in the superotemporal or inferotemporal quadrants. The conjunctiva is pushed to one side so that intact conjunctiva will cover the sutureless incision afterwards. A small-gauge, highspeed cutter is introduced and the lens fragments removed.5 Irrigation is titrated to maintain a stable anterior chamber.
While David Chang, M.D., has frequently
noted that bimanual vitrectomy with a separate limbal side-port infusion and high
cutting rate is accepted widely among surgeons, he also suggests the use of pars
plana
sclerotomy for the vitrectomy cutter. Once familiar with the pars plana
approach, the anterior segment surgeon will immediately grasp the advantages of
pulling vitreous gel away from the anterior chamber instead of drawing it forward
to the corneal incision. In addition, the ease of sutureless 25-gauge instrumentation
removes the obstacle of making a large sclerotomy.
Following vitrectomy, irrigation is maintained while cortical remnants are aspirated and the capsule cleaned as necessary. Finally, a cohesive viscoelastic is introduced through a corneal incision while continuous irrigation is still maintained, preventing further vitreous prolapse.
The haptics of the intraocular lens can then be inserted into the ciliary sulcus and the optic captured behind the capsulorrhexis, re-establishing a bicameral eye (Figure 1).6 Following removal of viscoelastic with irrigation and aspiration, the surgeon should ensure a vitreous-free anterior chamber by utilizing the staining technique discussed in the next section.
The Triamcinolone Assist
Scott Burk, M.D., and coauthors initially described the use of triamcinolone acetonide (Kenalog suspension, Bristol Myers Squibb) to stain the vitreous gel.7 They reported using 0.2 mL of injectable triamcinolone 40 mg/mL, passed through a 5 micron filter and rinsed with 2 mL of balanced salt solution. It was then resuspended in 5 mL of balanced salt solution and recaptured to thoroughly remove the preservative. The triamcinolone acetonide particles were ultimately resuspended in 2 mL of balanced salt solution and injected into the anterior chamber through a 27-gauge cannula. The triamcinolone acetonide particles were trapped on and within the vitreous gel, making it clearly visible. The visualization provided direct observation of vitreous behavior in various experimental settings and assisted surgeons intraoperatively in the identification and removal of vitreous in the anterior segment.
Currently, to stain vitreous gel in the anterior chamber, we combine 0.1-cc triamcinolone acetonide with 0.9-cc balanced salt solution in a 1.0-cc tuberculin syringe. We then irrigate this 10% dilution directly into the eye without filtering. Dr. Burk has noted that because there is no evidence that there is no clinical difference between the use of preservative-free vs. diluted triamcinolone for anterior vitrectomy, more data are required.8 The triamcinolone suspension clings to strands of vitreous in a characteristic fashion and makes complete removal significantly easier.
As an example, consider a case of endoscopic cyclophotocoagulation that was performed in a previously pseudophakic eye that had undergone a YAG capsulotomy years before. As always in such cases, we were concerned that vitreous could present during removal of the viscoelastic. In fact, a strand of vitreous clung to the aspiration tip. We carefully disengaged the strand with reflux and withdrew from the eye. Acetylcholine was then irrigated into the eye to constrict the pupil. As it happened, the pupil came down small and round, and the incision easily sealed with stromal hydration.
We then laid a fluorescein strip over the incision to check for a Seidel (this is a routine procedure we utilize at the end of every intraocular procedure). As the strip was withdrawn, we noticed a slight peaking of the pupil, suggesting the presence of a vitreous strand (Figure 2). Immediate triamcinolone staining revealed a substantial rope of vitreous running from the pupil to the incision. The strand was cut with Rappazzo scissors (Figure 3). Triamcinolone staining thus prevented a potentially significant complication.
|
|
|
Figure 3. Triamcinolone staining reveals a generous amount of vitreous gel in the anterior chamber. |
Innovative Applications
Phaco surgeons know that vitrectomy can save the day when complications arise. However, there are some other situations in which the advantages of vitrectomy might also spring to mind. These include secondary intraocular lens implantation,9 nanophthalmos,10 positive vitreous pressure with shallow anterior chamber,11 refractive lens exchange in high myopia,12 and routine pediatric cataract surgery.13 Surgeons should consider vitrectomy whenever the presence of vitreous gel presents a demonstrable risk.
In the case of nanophthalmos or shallow anterior chamber, the procedure may begin with an anterior chamber paracentesis incision, followed by the pars plana incision and vitrectomy (the paracentesis is performed first because it may be difficult to construct once the eye has become soft). The TSV 25-gauge trochar system (Bausch & Lomb, Rochester, N.Y.) provides one sutureless method of removing vitreous gel to allow subsequent deepening of the anterior chamber.14 The amount of vitreous removed is titrated by palpation of the intraocular pressure. Once the vitrectomy is complete, the anterior chamber is deepened with viscoelastic and the case proceeds as usual.
Converting a difficult situation into a familiar situation remains the goal of most approaches to challenging cataract cases. Pars plana vitrectomy and vitreous staining provide the anterior segment surgeon with valuable tools in a variety of cases. Adopting these relatively simple techniques will improve outcomes and allow greater flexibility in the operating room.
At the Casey Eye Institute at Oregon Health & Science University in Portland, I. Howard Fine, M.D., is a clinical professor, Mark Packer, M.D., is a clinical assistant professor and Richard S. Hoffman, M.D., is a clinical associate professor. Their practice, Drs. Fine, Hoffman & Packer, LLC, is located in Eugene, Ore.
Rosa Braga-Mele, M.D., is an assistant professor in the Department of Ophthalmology, Faculty of Medicine, at the University of Toronto, Canada. She is also the director of the Cataract Unit and Surgical Teaching at Mount Sinai Hospital, Toronto.
References
1. Fine IH, Hoffman RS, Packer M. Optimizing refractive lens exchange with bimanual microincision phacoemulsification. J Cataract Refract Surg. 2004;30:550-4.
2. Brauweiler P. Bimanual irrigation/aspiration. J Cataract Refract Surg 1996; 22:1013-1016
3. Smith JH. Teaching bimanual microincision cataract surgery in a residency program. Symposium on Cataract, IOL and Refractive Surgery, ASCRS; April 19, 2005, Washington, DC.
4. Blumenthal M. Use and results using the new ACM. Symposium on Cataract, IOL and Refractive Surgery, ASCRS; April 18, 2005, Washington, DC.
5. Chalam KV, Shah VA. Successful management of cataract surgery associated with vitreous loss with sutureless small-gauge pars plana vitrectomy. Am J Ophthalmol. 2004;138:79-84.
6. Gimbel HV, DeBroff BM. Intraocular lens optic capture. J Cataract Refract Surg. 2004;30:200-6.
7. Burk SE, Da Mata AP, Snyder ME, Schneider S, Osher RH, Cionni RJ. Visualizing vitreous using Kenalog suspension. J Cataract Refract Surg. 2003;29:645-651.
8. Burk SE, Mata AP, Osher RH, Cionni RJ. Triamcinolone-Assisted Anterior Vitrectomy. http://www.ophthalmic.hyperguides.com/. (Accessed May 31, 2006).
9. Jacobi PC, Dietlein TS, Jacobi FK. Scleral fixation of secondary foldable multifocal intraocular lens implants in children and young adults. Ophthalmology. 2002;109:2315-24.
10. Chan FM, Lee L. Nanophthalmic cataract extraction. Clin Experiment Ophthalmol. 2004;32:535-8.
11. Chalam KV, Gupta SK, Agarwal S, Shah VA. Sutureless limited vitrectomy for positive vitreous pressure in cataract surgery. Ophthalmic Surg Lasers Imaging. 2005;36:518-22.
12. Uhlmann S, Wiedemann P. Refractive lens exchange combined with pars plana vitrectomy to correct high myopia. Eye. 2006 Feb 3; [Epub ahead of print]
13. Biglan AW. Modification of the high-speed vitrectomy system TSV 25 for pediatric cataract surgery. J Cataract Refract Surg. 2005;31:2257-60.
14. Braga-Mele R. The role of sutureless posterior vitrectomy in challenging anterior segment surgery. XXII Congress of the European Society of Cataract and Refractive Surgeons. Paris, 18-22 September 2004.