feature
Aggressive Treatment of Post-LASIK Dry Eye
Early
and aggressive therapy produces rapid improvement.
BY
WILLIAM TRATTLER, M.D.
Nearly four in 10 Americans suffer from symptoms of dry eye,1 one of the most common complaints seen by eye doctors; accounting for nearly one-fourth of all office visits.2,3 The condition often occurs after LASIK surgery, even in individuals with no history of the disease.4 The following situation has been seen a few times in our clinic in terms of both presentation and resolution with aggressive therapy.
|
|
|
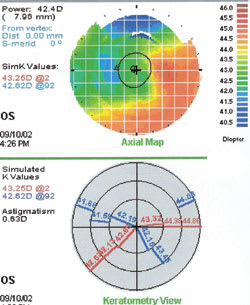
Figure 1. Eighteen months following LASIK surgery. |
Case History
A 23-year-old male underwent LASIK surgery and reported very good visual results initially. Eighteen months later he noted a decrease in vision, which was corrected with glasses. Three years later, he developed post-LASIK ectasia of the left eye (Figures 1 and 2), and was fitted with a corrective contact lens.
No old records were available for the patient since the corporate laser center had closed operations, so we could not determine preoperative risk factors for ectasia, e.g., keratoconus, forme fruste keratoconus, pellucid marginal degeneration, excessively thin preoperative corneal thickness and/or deep ablation leaving a thin residual stromal bed.
The patient noted improved vision with a contact lens, but subsequently reported contact lens intolerance, including irritation when wearing the lens and blurred vision. We sought to determine whether the cause of the intolerance was due to advanced corneal ectasia or dry eye.
Patients who undergo LASIK are at increased risk for developing dry eye. The causes can be multifactorial. For example, the LASIK procedure severs the corneal nerves, which can take from months to years to completely regenerate.5 Additionally, patients with complaints of post-LASIK dry eye often have meibomian gland dysfunction, which leads to poor tear film quality. For patients with post-LASIK ectasia, there is the additional challenge of the irregular shape of the cornea, which can exacerbate dry eye in patients with an abnormal tear film layer.
Examination/Treatment
An examination revealed significant signs of dry eye, including punctate staining with fluoroscein dye and lissamine green dye (Figure 3), abnormally viscous meibomian gland secretion, and low Schirmer's test score. Evaluation of the tear film also revealed a very low tear film lake.
In cases such as this, we recommend early and aggressive therapy for dry eye to halt its progression, and allow the patient to resume contact lens wear as soon as possible. We started five treatment modalities on the first visit:
|
|
|
Figure 2. Five years post-LASIK, demonstrating ectasia. |
1. Restasis (cyclosporine, Allergan) 0.05% eye drops b.i.d. to increase tear production, increase goblet cell density and improve meibomian gland function.6 Studies have also shown that Restasis can improve contact lens tolerance.7
2. Pred Forte (prednisolone acetate) eyedrops q.i.d. for the first week, to provide initial and rapid-acting anti-inflammatory therapy in conjunction with the anti-inflammatory affects of Restasis. During this week, the patient could not wear the contact lens.
3. Punctal plugs (Parsol, Odyssey Medical) to increase tear volume on the ocular surface.
4. Refresh Liquigel lubricant eye drops (Allergan) t.i.d. and Genteal Gel (Novartis Ophthalmics) in each eye at bedtime, to lubricate the ocular surface during the day and provide extended lubrication at night, respectively.
5. Oral supplements of omega-3 fatty acids to help with the quality of meibomian gland secretion.
Follow Up
The patient's dry eye signs and self-reported symptoms improved over the first 2 weeks. The punctate staining was significantly reduced. The patient was able to restart his contact lenses again, and has showed improved contact lens tolerance. The patient continues using Restasis b.i.d., Refresh Liquigel as needed and oral omega-3 fatty acid supplements. Currently at 8 weeks follow-up, the patient continues to wear his contact lens comfortably to correct for the post-LASIK ectasia.
Discussion
The goals of treatment for dry eye include reducing or alleviating signs and symptoms, maintaining visual function, reducing or preventing structural damage and preventing progression of the disease.8 Dry eye diagnostic and management guidelines have been published by the American Academy of Ophthalmology (AAO)8 and the American Optometric Association,9 but they are not in widespread use.
|
|
| Figure 3. Punctate staining using fluorescein dye. |
A survey found that 65% of specialists use no dry eye treatment guidelines but were interested in guidelines that used a practical treatment algorithm.10 To address this need, an international task force (ITF) of dry eye experts recently developed treatment guidelines recommending: 1) the approach to therapy should primarily be determined based on the severity of symptoms and signs; 2) the patient's response to treatment should be determined and therapy adjusted as needed; and 3) anti-inflammatory therapy should be used regardless of the level of clinically apparent inflammation.11 The ITF guidelines recommend a continuum-of-care approach based on assessing dry eye severity level, and that if symptoms do not improve, treatment components at the next level of severity should be added. As shown in the Table, treatment components include artificial tears, various anti-inflammatory medications and surgical procedures.
Given this patient's high degree of dry eye associated discomfort and contact lens intolerance, we assessed him at a severity level of 3 and pursued aggressive treatment with multiple modalities. His rapid response not only provided symptomatic relief and at least partial resolution of dry eye, but also allowed him to resume daily functioning at work and in other environments.
William Trattler, M.D. is the director of cornea at The Center For Excellence In Eye Care, in Miami, FL. Dr. Trattler completed his Ophthalmology residency at the University of Pennsylvania's Scheie Eye Institute, and performed a cornea and refractive surgery fellowship at Southwestern Medical Center in Dallas. Dr. Trattler has been involved in a number of phase 3 and phase 4 dry eye treatment studies.
|
Table. Treatment of Dry Eye Based on Severity Level11 |
||
| Severity Level | Signs and Symptoms | Recommended Treatment |
| 1 |
� Mild to moderate symptoms, no signs � Mild to moderate conjunctival signs |
Patient counseling, preserved
tears, environmental management,control
allergy, use of hypoallergenic products, water intake
If no improvement, add Level 2 |
| 2 |
� Moderate to severe symptoms � Tear film signs � Mild corneal punctate staining � Conjunctival staining � Visual signs |
Unpreserved tears, gels,
ointments, cyclosporine A, topical steroids, secretagogues, nutritional
support (e.g., flax seed oil, fish oil) If no improvement, add Level 3 |
| 3 |
� Severe symptoms � Marked corneal punctate staining � Central corneal staining � Filamentary keratitis |
Tetracyclines, punctal plugs If no improvement, add Level 4 |
| 4 |
� Extremely severe symptoms � Severe corneal staining � Corneal erosions � Conjunctival scarring |
Systemic anti-inflammatory therapy, moisture goggles, N-acetylcysteine, punctal cautery, surgery |
References
1. Multi-sponsor surveys, Inc. Gallup study of dry eye sufferers. Princeton, NJ, August 2004.
2. Hikichi T, Yoshida A, Fukui Y, et al. Prevalence of dry eye in Japanese eye centers. Graefe's Arch Clin Exp Ophthalmol. 1995;233:555-558.
3. Doughty MJ, Fonn D, Richter D, et al. A patient questionnaire approach to estimating the prevalence of dry eye symptoms in patients presenting to optometric practices across Canada. Optom Vis Sci. 1997;74:624-631.
4. De Paiva CS, Chen Z, Koch DD, et al. The incidence and risk factors for developing dry eye after myopic LASIK. Am J Ophthalmol. 2006;141:438-445.
5. Calvillo MP, McLaren JW, Hodge DO, Bourne WM. Corneal reinnervation after LASIK: prospective 3-year longitudinal study. Invest Ophthalmol Vis Sci. 2004;45:3991-3996.
6. Perry HD, Doshi-Carnevale S, Donnenfeld ED, Solomon R, Biser
SA, Bloom AH. Efficacy of commercially available topical cyclosporine A 0.05% in
the treatment of meibomian gland dysfunction. Cornea. 2006;25:
171-175.
7. Hom MM. Use of cyclosporine 0.05% ophthalmic emulsion for
contact lens-
intolerant patients. Eye Contact Lens. 2006;32:109-111.
8. American Academy of Ophthalmology Cornea/External Disease Panel. Dry Eye Syndrome Preferred Practice Pattern. American Academy of Ophthalmology, San Francisco, Calif., 2003.
9. American Optometric Association. Optometric clinical practice guideline care of the patient with ocular surface disorders. Available at: http://www.aoa.org/documents/cpg-10.pdf. Accessed February 16, 2006.
10. Behrens A, et al. ITF guidelines. Cornea. in press.
11. McDonnell PJ, Doyle JJ, Stern L, Chuck RS, Behrens A, for the Dysfunctional Tear Syndrome Group. A modified delphi technique to obtain consensus on the treatment of dysfunctional tear syndrome. Presented at: ARVO; April 28, 2004.