feature
EMR for the Smaller Practice
With
fewer staff, physician-related efficiencies become the key goal.
BY JERRY HELZNER, SENIOR EDITOR
If you are in solo practice and contemplating retirement sometime within the next 5 years, this article is probably not for you. It is highly unlikely that you will be interested in making the significant investment to convert your paper charts to an electronic medical records (EMR) system this late in your career.
But if you plan on maintaining, growing, or even selling your practice, it is important that you become as informed as possible on the costs, benefits and potential pitfalls involved in initiating an EMR installation.
Why should you be interested in EMR, and especially why should you be thinking about installing an EMR system now?
Several factors have stirred recent interest in ophthalmology practices converting to EMR. These factors include major advances in EMR technology, the implementation of HIPAA regulations, increasing pressure from payers for practices to go electronic, and the realization by many practices that conversion to EMR can create numerous efficiencies, increase profitability, raise the level of patient satisfaction and generate data that can help in evaluating and improving outcomes.
Given the pressures to go electronic that already exist — and the fact that some form of pay-for-performance, with all of its accompanying data-documentation requirements, will be adopted by CMS in the not-too-distant future — some respected healthcare analysts are now predicting that even smaller medical practices will have to install EMR in the next 5 to 10 years or face the prospect of not being able to operate profitably.
This article will offer guidance to smaller practices whose principals are now deciding whether to make the major investment in time and money required to implement an EMR installation.
Physician-Related EMR
Practice administrators, EMR consultants and vendors agree that the ophthalmology-related demand for EMR that has developed in the past 2 years will continue to grow. The good news is that with fewer than 20% of ophthalmology practices currently using EMR, major vendors are sensing opportunity in this market and are making investments to improve their product offerings. This is especially good news for smaller practices because these practices generally do not have the in-house expertise to develop their own content and must primarily depend on vendors and consultants to steer them in the right direction.
|
|
|
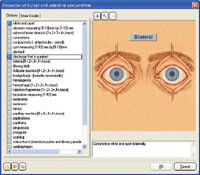
Specific examination templates, such as this one from MediNotes for the conjunctivae, create easy-to-retrieve patient records. |
Clearly, it has primarily been large general ophthalmology practices that have adopted EMR until now. Because some of these practices have hundreds of staff members in multiple locations serving thousands of patients, implementation of EMR has enabled a number of these practices to generate staff-related efficiencies that are allowing payback on 7-figure investments in 18 months or less. For example, EMR virtually eliminates the estimated $3-$6 it costs to pull each paper chart.
But smaller practices, with their smaller staffs, cannot generate the staff-related efficiencies that large practices can achieve. For this reason, most smaller practices, until now, have been reluctant to make what is usually a six-figure investment in an EMR installation, combined with the major training effort that is necessary for the successful implementation of EMR.
"The key issue for smaller practices is the willingness of the doctor to use EMR," says EMR consultant Ron Sterling of Sterling Solutions in Silver Spring, Md. "In larger practices, a number of benefits can be generated 'around' the doctor, but in a smaller practice there are few benefits around the doctor. To select an EMR system, the practice should develop a list of requirements built around the four key areas of EMR: image management, practice workflow, charting patient visits and patient service."
The Benefits of EMR
For smaller practices that purchase a proven, ophthalmology-specific system from a reliable vendor, EMR can improve revenue, cut expenses and improve patient service. The more efficient response to patients' needs is almost always noticed by patients, who credit the practice with having "state-of-the-art" technology. Practices report that having EMR has resulted in many word-of-mouth referrals from impressed patients.
Revenue enhancement is available through improved E&M coding, as well as the virtual elimination of missed charges. Expenses for dictation and medical records can be dramatically cut through the use of an EMR. Patient service and physician productivity can be improved through instantaneous access to the patient medical record. For example, a patient's phone call can be immediately addressed because the doctors and staff can call up the patient's medical record to access patient information and document the patient's issue. If necessary, a follow-up note can be directly routed to staff and doctors through the EMR.
Smaller retina practices should focus on creating physician-related efficiencies in areas such as drawing, creating letters to referring physicians, interfacing with diagnostic equipment, and image storage/retrieval. These capabilities should be available "out of the box," says Sterling, as here again, smaller practices do not usually have the resources or doctor time to develop customized retina content for the practice.
Smaller ophthalmology practices of all types that are seeking to grow should be looking ahead to the next decade and the huge, aging cohort of about 40 million "baby boomers" who will almost certainly create additional patient volume for practices that are prepared to handle it. Installing EMR in the near future will enable those practices to operate efficiently as patient volume increases and the practice grows.
Smaller Practices have Converted
Ophthalmology Management asked several ophthalmologists who operate small-to-mid-size practices to comment on the benefits they are deriving from their EMR installations. Many practices choose EMR systems that are designed to be able to interface with most existing practice management systems through what is called the HL7 protocol. This capability often spares a practice the expense of replacing its practice management system when it installs EMR.
Following are the ophthalmologists' comments:
"Our MediNotes EMR has allowed me to offer my patients state-of-the-art document management as their medical records custodian," says Michael Loeffler, M.D., of Lighthouse Point, Fla. "Their charts are now neat, organized and always available for all the staff to access at any time with no more lost charts. All chart entries are legible and communication between doctors has been greatly facilitated, as well as being more efficient, as referring physicians get reports almost immediately using the reporting software contained in our system.
"I no longer pay any transcription costs at all," continues Dr. Loeffler. "I have created office space where my large chart rack used to be and I have been able to lighten my payroll by no longer needing a filing clerk. You do the math. I was able to recover my investment within a year."
Kenneth J. Rosenthal M.D., F.A.C.S. surgeon director for Rosenthal Eye and Facial Plastic Surgery, Great Neck, N.Y., and a NextGen user, says "Having electronic records is at least as important, if not more so, for the solo practice as it is for the larger group practice. In the era of complex and ever-changing compliance requirements, electronic records ensure that a consistent, legible and accurate record of patients' medical encounters is created. Additionally, they allow for efficiencies in data collection and recording not afforded by paper records.
"An example of this exists in the ability to collect data from diagnostic instruments and incorporate them into the record," Dr. Rosenthal continues. "In some cases, the data is quantitative (e.g. refractive data) and the automatic population of data fields in the medical record eliminates the possibility of transcription and clerical errors and allows rapid completion of the tests. Tests that require interpretation can be flagged on a list and completed. Tests that require follow up can likewise be listed on a reminder list. The ability to graph serial test values is also a unique feature of the EMR. For example, I can summarize glaucoma patients' IOPs in a graph and even superimpose the time line for their medications. This is extremely valuable, not only for clinical assessment and decision making, but as a patient teaching tool, it can also be helpful in assuring medication compliance.
"Also, as a frequent lecturer, I am out of the office a great deal of the time, during which there is no physician in the office to handle patient problems. By having access to my patients literally from anywhere in the world, I can review patient records, and handle their telephone inquiries at any time. This ensures that I have as much information about a patient as possible when making decisions about their care out of the office," Dr. Rosenthal concludes
And, finally, Lee Shettle, D.O., of Largo, Fla., a MediNotes user, says, "Our EMR system provides me with the ability to select specific line-item data from my medical notes and view this information on one screen for specific diseases. I am able to quickly and accurately assess a patient's disease process. Our EMR allows me the ability to categorize data in a layout that is specific to my practice patterns, not one that is written by a programmer.
"With update software, I will be able to view visual fields and other reports side by side to better treat my patients, instead of flipping through old records attached to binders in a folder," adds Dr. Shettle. "I can then show my patients their results on the flat thin screen monitor in a very professional manner. Most of all, I know that I am documenting the patient's visit thoroughly because I can set the attributes behind the scene, so to speak, which reminds me to document certain data points before I digitally sign the note."
What You Should Know
Physicians and administrators of smaller practices usually have some key questions as they contemplate a conversion from paper records to EMR. This short Q. and A., with answers provided by Ron Sterling, should help answer these questions:
Q: What should I be looking for in a vendor?
A: Smaller practices need to ensure that the vendor will have the resources to guide you through the implementation process, as well as support your practice going forward. Though the practice may be small, you need to have the support and response mechanism in place to assure that you can get access to your patient records.
Q: What about cost?
A: In general, practices are looking at $25,000-$50,000 per doctor. For example, you will have to give each person in the practice access to the EMR, and you will want to invest money in components that are protected from a catastrophic failure.
Q: How can the investment pay for itself?
A: For the smaller practice, benefits from office efficiencies may be difficult to attain. Regardless of how efficient your office is, you will need someone to greet patients and answer the phones. Additionally, most practices need even more help during the initial phases or EMR activation.
Paybacks from EMR for the small practice will occur from decreased transcription expenses almost immediately, and a lower level of medical record expenses starting 6 months after the system "goes live." Other paybacks will come from more effective coding and the tracking of all services provided to a patient.
Q: Will EMR increase patient satisfaction?
A: EMR absolutely improves patient satisfaction because the doctor and staff can instantaneously access the medical record to address an issue. Patients' anxiety will be decreased when they can get an answer to a question or clarify an issue in a shorter time frame. Indeed, some studies are showing that an EMR and electronic support for patient services are starting to affect patients' choice of medical practices.
Q: How should we approach staff training?
A: Staff training should include training on the EMR system, as well as training on the new procedures to be used in the practice. Note that practices should allow plenty of time for training and testing to insure that you minimize the effect on patients.
Q: Will we need an outside consultant?
A: Implementing an EMR requires a variety of skills that few smaller practices have. From complex computer issues to software setup and practice workflow, practices need to redesign themselves to use the EMR. Lacking such expertise, practices should consider the project management and subject matter expertise that will be needed to successfully deploy an EMR.
Q: How long should it take to go from beginning implementation of EMR to achieving a well-functioning system?
A: After you sign a contract, it will take at least 4 months to get started using the EMR. A well-functioning system can be achieved when the practice fully acclimates to the EMR in another 3 to 6 months. However, many practices fail to achieve a well-functioning system due to inappropriate products, poor EMR setup and lack of will. EMR implementation is a difficult process, because the EMR affects every patient and employee, every practice process and action. Practices implementing EMR have to realize the effect of the EMR and seriously consider the effect of the change to their practice and patients.