feature
New Concept for Refractive Surgery:
Corneoplastique
A
synergistic approach to refractive correction may help patients who are not candidates
for standard procedures.
BY
ARUN C. GULANI, M.D.
Arun C. Gulani, M.D., has experience with over 30 surgical techniques in refractive surgery. In his practice, he performs all levels of lamellar corneal surgery from anterior (superficial, mid, deep) to posterior endothelial transplants and artificial cornea, sutureless amniotic membrane resurfacing and synthetics, as well as the full spectrum of laser vision and IOL procedures.
Dr. Gulani compiled all his approaches for refractive surgery with the above-mentioned base surgeries and concluded that most patients can be candidates for refractive surgery with a possible goal of unaided emmetropia. He proposes that the cornea can be used as the final fine-tuning platform to achieve the best possible uncorrected visual acuity. This article describes a holistic approach to refractive surgery that has allowed him to provide his patients with good visual acuity irrespective of their causative pathology.
Dr. Gulani also acknowledges the contributions of Lee T. Nordan, M.D., to the development of the technique that he describes.
In my practice, I routinely see patients who have been referred or who seek a second opinion refractive surgery or LASIK complication management. These patients typically have either undergone or are considering traditional treatment or surgical procedures that are intensive and require prolonged rehabilitation periods, all while providing no promise of excellent unaided vision.
The Corneoplastique Procedure
To address the challenging issues that these patients present, I have developed a protocol that utilizes a spectrum of surgical techniques, which I call Corneoplastique (Gulani Vision Institute). These techniques are usually brief, topical, aesthetically appealing and visually promising, and can be used either singly or in combination with one another, either directly consecutive or in stages.
Simply put, the Corneoplastique protocol builds the cornea or ocular refractive status by implementing a strategy of clear visual axis and final corneal reshaping. Thus, the art of blending the full spectrum of ocular surface and corneal surgery (sometimes in combination with intraocular surgery) in a therapeutic approach either before (to prepare the cornea) or after laser vision surgery (to repair the cornea) is the core function of Corneoplastique.
These surgical techniques involve lamellar corneal procedures, amniotic membrane resurfacing, Tiseel fibrin glue (Baxter Healthcare Corp., Deerfield, Ill.) and synthetic inserts, such as Intacs (Addition Technology, Sunnyvale, Calif.), and for the final step: fine-tuning with an excimer laser.
The Corneoplastique approach to refractive correction is in contrast to the more extensive standard surgical techniques such as PK where, in most cases, the final unaided visual outcome is less than optimal for the patient. However, standard surgeries can always be used in conjunction or as back up with the Corneoplastique approach due to its synergistic nature and the surgeries' proven track record.
Patient Selection and Preoperative Screening
Patients who are presented with such a spectrum of options for their individual ocular status are not only impressed, but feel reassured that a specific surgical plan is being customized for them. It is important to offer patients not only a variety of options, but also to take into account their best interests. By properly educating patients as to what their options are based on their individual needs and co-existing conditions, surgeons can manage patient expectations, especially when patients hold preconceived and incorrect ideas about what a particular procedure can accomplish.
Patients who may be candidates for a Corneoplastique procedure include those who are contraindicated for traditional corneal laser surgery because of pre-existing conditions such as corneal scarring from previous surgery, trauma, healed corneal ulcers and previous infections, ectasia, pterygiums (advanced and recurrent), herpes, and corneal degenerations and dystrophies. Additionally, patients who are contraindicated because of previous cataract surgery, corneal transplants, retinal surgery, glaucoma surgery or radial keratotomy are also candidates for this procedure. The true contraindications for this approach would include uncontrolled or active pathology such as retinal disease, neurological disease or glaucoma.
For diagnostic screening, I use the Pentacam (Oculus, Lynnwood, Wash.). The Pentacam is the world's first Scheimpflug rotating camera that images the eye on different angles and allows for the surgeon to look at the complete anterior segment. The Scheimpflug system involves achieving a higher depth of focus by moving the picture/film and objective plane (which are parallel in normal cameras) so they meet at the point of intersection. The Pentacam has the ability to reconstruct the patient's cornea and, more importantly, its relation to associated structures in dynamic anatomy. This complete information is important because my concept of Corneoplastique uses the entire anterior segment and the cornea as a platform for visual rehabilitation.
Preoperative and Postoperative Regimen
The preoperative and postopoperative regimen is no different than what is used for traditional corneal laser surgery. I use a steroid and antibiotics drops for 2 weeks.
My final excimer laser application involves the use of the Star S4 VISX laser (Advanced Medical Optics [AMO], Santa Ana, Calif.) to sculpt the cornea for the desired refractive effect. I am interested in the future uses and modifications of femtosecond lasers, such as the IntraLase FS (IntraLase, Irvine, Calif.) and the Da Vinci femtosecond laser (Zeimer Ophthalmic, Port, Switzerland), and have looked at some new laser technologies abroad.
Corneoplastique would be a perfect match for femtosecond lasers, as it would expand the indications of laser vision surgery, not only from the point of view of including previously unacceptable cases, but also to correct inadequate or complicated outcomes of traditional LASIK applications.
Given that any technique used in the Corneoplastique methodology is topical and brief, the complication rate is low. To manage a complication that might occur, I would recommend retreatment with either re-surgery or conventional surgery such as penetrating keratoplasty
Better Visual Outcomes
The visual recovery period for this surgical approach is short, and in many cases, vision has been restored to 20/20. Unaided emmetropia is the goal for any Corneoplastique procedure. It is important to note again that Corneoplastique may be performed in stages, and that if the patient is happy with the result at any stage, the surgeon should adapt the surgical plan accordingly. Patient satisfaction is the most important consideration in this technique. While LASIK on the virgin eye may sometimes achieve 20/15 or 20/10 vision, patients who undergo a Corneoplastique procedure are thrilled to achieve even 20/40 vision, because they would have not been considered candidates for refractive correction previously.
The Corneoplastique technique can be utilized for practically any ocular condition, provided visual potential exists and the patient has no ongoing or uncontrolled visually debilitating pathology.
Arun C. Gulani, M.D., is founding director of Gulani Vision Institute in Jacksonville, Fla. He can be reached at 904-296-7393 or gulanivision@gulani.com.
|
Case 1 |
Case 2 | Case 3 | Case 4 |
|
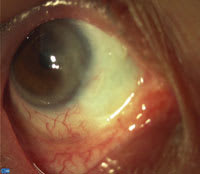
Patient
presented with advanced recurrent pterygium reaching the corneal apex with cosmetic
and visual compromise (Figures 1 and 2). |
Patient presented with extensive ocular surface
and corneal scarring with vascularization following cement burns over 20 years
ago (Vision: Hand motion OD) (Figures 3 and 4). Stage One: Amniotic membrane surface reconstruction covering sclera, cornea and fornices with resultant white and cleared sclera and decreased density of corneal scar. Stage Two: Through the lesser corneal scar, one could visualize an advanced cataract and corectopia (pupil updrawn superior-temporally). Phacoemulsification was undertaken through poor corneal visibility and an Acrysof IOL (Alcon, Fort Worth, Texas) successfully implanted in the bag. The capsulorrhexis was designed to cover the area of the missing pupil superior-temporally. Stage Three: This patient underwent excimer laser corneal surgery
with result of uncorrected 20/40 vision. |
Chemical
burns with corneal and conjunctival scars, psuedopterygium etc. Referring surgeon
had already performed cataract surgery on this eye. Vision Cf5ft. Stage 1. Amniotic membrane transplant to correct the ocular surface and retrieve the function and appearance (Figure 5). Vision 20/100. Stage 2. Lamellar keratectomy with amniotic membrane resurfacing the cornea – clearer cornea and vision 20/80 (Figure 6). Vision with RGP contact lens is 20/40. Through the clearer cornea we could now see posterior capsular opacity. Stage 3. YAG laser capsulotomy (Figure 7). Vision 20/20 with RGP contact lens. Stage 4. Excimer laser PRK with mitomycin- Uncorrected 20/15 (Figure
8). |
Patient had aphakic decentered epikeratophakia
nearly two decades ago with best-corrected 20/200 vision. Stage 1. Removal of her epi lenticle (Figures 9 and 10). Stage 2. Insertion of secondary IOL (Figure 11). Uncorrected vision
20/25.
|