LASIK: Avoiding
Dry Eye and Corneal Complications
Patients' complications can be lessened by
understanding the ailment and managing corneal issues.
BY RENéE SOLOMON, M.D., AND
ERIC DONNENFELD, M.D.
Dry eye following LASIK is arguably the most common problem facing refractive surgeons and their patients today.1-4 Virtually all patients experience dry eye at least temporarily following LASIK. Therefore, to prevent and manage this common disorder it is important to have an understanding of the pathophysiology of dry eye after LASIK. This includes an understanding of the relationship and interaction between inflammation, sensory denervation and the essential fatty acid pathways. In addition, there is a second form of dry eye related to LASIK in the form of corneal erosions.
Inflammation
The importance of inflammation in the pathogenesis of dry eye disease has been elucidated over the past decade. Decreased tear production and tear clearance lead to chronic inflammation of the ocular surface. This inflammatory response consists of activated T-lymphocyte cellular infiltration of the ocular surface, with increased expression of adhesion molecules and inflamed cytokines, leading to increased concentrations of inflamed cytokines in the tear fluid, and increased activity of matrix-degrading enzymes such as MMP-9 in the tear fluid.5 Significant positive correlation has been observed between the levels of inflammatory cytokines in the conjunctival epithelium and the severity of ocular irritation symptoms, corneal fluorescein staining and conjunctival squamous metaplasia in patients with Sjögren's syndrome keratoconjunctivitis.6,7 Reports of clinical efficacy of anti-inflammatory therapies for treatment of dry eye disease provide direct proof of the principle that inflammation is involved in the etiology of dry eye disease. Patients seeking refractive surgery are often pre-selected for dry eye because of their contact lens intolerance. Carefully screening these patients for dry eye preoperatively allows the clinician the opportunity to treat the underlying disorder with immunotherapy such as Restasis (cyclosporine 0.05%, Allergan) prior to LASIK. Pre-treating dry eye with Restasis has been shown to improve surgical outcomes and reduce the incidence of postoperative dry eye.
Sensory Denervation
The recognition that the ocular surface and lacrimal glands function as an integrated unit represents a major advance in the understanding of dry eye. Communication between the ocular surface and lacrimal glands occurs through a sensory/autonomic neural reflex loop.8,9 The sensory nerves innervating the ocular surface connect with efferent autonomic nerves in the brain stem that stimulate secretion of tear fluid and proteins by the lacrimal glands. Ocular surface sensitivity has been found to decrease as aqueous tear production and clearance of tears from the ocular surface decrease. This decrease in surface sensation in turn exacerbates dry eye because sensory-stimulated reflex tearing is decreased, resulting in decreased ability of the lacrimal glands to respond to ocular surface insults. Thus, a self-perpetuating cycle between the lacrimal glands and the ocular surface is created.8,9 The anesthetic cornea created by the LASIK flap and photoablation will create or worsen pre-existing dry eye syndrome by reducing the afferent pathways from the cornea to the brainstem, thereby reducing the efferent signal from the brainstem to the lacrimal glands to produce tears. Steven E. Wilson, M.D., has reported that even with unaltered tear production post-LASIK, there is corneal staining, leading him to postulate that neurotrophic keratitis rather than dry eye may be responsible for some of the corneal changes following LASIK.10
|
|
|
|
Figure 1. Effects of eicosapentaenoic acid (EPA) and omega-3 fatty acids on the ocular surface. |
|
|
|
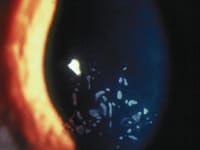
| Figure 2. Epithelial basement membrane disease in a patient who was a candidate for LASIK. |
Essential Fatty Acid Pathways
The essential fatty acid metabolic pathways are dynamic, complex and interrelated. Levels of certain omega-3s, for example, can influence the metabolism of omega-6s. The most important example of the interrelationship is the activity of eicosapentaenoic acid (EPA). EPA inhibits the arachidonic acid inflammatory cascade. EPA also competitively inhibits the conversion of dihomo-g-linolenic acid (DGLA) to arachidonic acid (AA), and, in doing so, promotes the conversion of DGLA to prostaglandin E1 (PGE1). This is desirable because PGE1 has anti-inflammatory properties that help to reduce meibomitis and associated ocular surface inflammation.11,12 More importantly, PGE1 acts on G protein-coupled receptors designated E-prostanoid or "EP" receptors. Specifically, PGE1 binds to EP2 and EP4 receptors to activate adenylate cyclase to increase cyclic adenosine monophosphate (cAMP).13 PGE1 has been shown to stimulate aqueous tear production in rabbits,14 and cAMP has been shown to stimulate aqueous tear secretion in dry eye.15 By decreasing inflammation and augmenting the oil and water layers of the tear film, omega-3 supplementation with EPA and DHA-enriched flaxseed oil may provide the foundation for a broad spectrum dry-eye treatment regimen (Figure 1). In patients with meibomian gland disease who are interested in refractive surgery or in patients who have undergone previous LASIK, nutritional supplementation with oral flaxseed oil and fish oils rich in EPA may improve both the lipid and aqueous component of the tear film. This may improve surgical outcomes by stabilizing the tear film, reducing epithelial defects and promoting normal wound healing.
LASIK and Corneal Erosions
While dry eye is one aliment to consider preoperatively, another prospective area to evaluate before LASIK is corneal epithelial adhesion to the anterior stroma. This can be a potentially relevant variable to be considered in candidates for refractive surgery. Large epithelial defects and/or epithelial sloughing occur in LASIK because of a poorly adherent corneal epithelium.16 Epithelial defects dramatically increase the incidence of non-keratome related LASIK complications, including diffuse intralamellar keratitis (DLK), flap folds, epithelial ingrowth and infectious corneal ulceration. Among the most important variables in deciding between LASIK and a surface ablation is the extent of corneal epithelial adhesion and the presence or absence of epithelial basement membrane dystrophy.
The basal layer of the corneal epithelium adheres to the basement membrane and Bowman's layer through a series of inter-related structures known as the adhesion complex.17,18 These structures, which function as welds, are well arranged and include intracellular keratin filaments that connect to the outer layer of hemidesmosomes, basal laminae and an anchoring network, which penetrates about 2 mm in the superficial stroma. The anchoring network is composed of anchoring filaments, anchoring fibrils and anchoring plaques. Each of these elements has a specific biochemical component.
Edgar M. Espana, M.D., and colleagues used immunofluorescence staining with monoclonal antibodies against laminin 5, collagen VII and beta integrins in epithelial flaps created in cadaver eyes, as well as in epithelial flaps obtained during LASEK cases that were converted to standard PRK.19 Based on immunofluorescent staining, they concluded that the cleavage plane of the ethanol-induced corneal epithelial flap is located between the lamina lucida and the lamina densa of the basement membrane. Various other types of junctional complexes exist within the cornea, such as tight junctions (superficial epithelium and endothelium), gap junctions (between most corneal cells), and desmosomes.20 Transmission electron microscopy has been used to study these structures.
The basal epithelial cells of the cornea actively secrete their own basement membrane. The basement membrane provides stability and support for keeping the epithelium healthy, even when it is exposed to the everyday trauma of blinking. Normal corneal epithelium basement membrane is generally less than 100 nanometers thick and has a well-developed anchoring complex. However, certain conditions, such as epithelial basement membrane dystrophy (EBMD), (Figure 2) recurrent erosions and diabetes are associated with a thicker multi-laminated basement membrane with no evidence of a normal anchoring complex.21,22
A thicker, multi-laminated basement membrane was seen in a series of epithelium specimens obtained from eyes that had epithelial sloughing during LASIK and in cases of EBMD that had planned surface ablation (PRK).23,24 It is important to note that in these cases of sloughing, no slit lamp signs of map, dot or fingerprint dystrophy were seen. PRK cases with normal cornea served as controls; in these, a very thin basement membrane was evident with the remaining anchoring complex attached.
The most common corneal dystrophy is EBMD.23 It is also known as map-dot fingerprint dystrophy because of the classic findings seen on slit lamp examination. EBMD is commonly associated with painful, spontaneous, recurrent corneal erosions, which usually occur upon awakening. These painful episodes are characteristically transient, lasting for a few minutes; however, they can persist for hours or even days and may be associated with blurred vision. Commonly, EBMD in the visual axis is associated with loss of best-corrected visual acuity. A second variety of recurrent erosions occur after organic corneal trauma.25
Flap Complications
Epithelial defects can occur during the creation of the LASIK flap, and this represents one of the most common flap complications associated with LASIK. Epithelial defects have been estimated to occur in 1.6% to 5% of cases.16,26 An epithelial defect is not considered a serious flap complication, and the procedure can be concluded with laser ablation. However, epithelial defects increase patient discomfort, prolong recovery time, and increase the risk for several other postoperative complications.16 For example, the relative risk of developing DLK is increased up to 24 times with an epithelial defect.27,28 Infection, epithelial ingrowth, recurrent corneal erosions, flap melts, irregular healing patterns associated with loss of BCVA and undercorrection are also associated with epithelial defects related to the creation of the flap.16, 29-33 The size of the epithelial defect may be important, with larger defects having a greater risk of complications. With regards to flap melts, they have very rarely been associated with flap dislocation and the use of a topical NSAID.34
Other Causes of Erosions
Mechanical factors related to the microkeratome also increase the risk of epithelial defects, but epithelial slough is generally related to abnormalities on the adhesion complex of the corneal epithelium to its basement membrane. EBMD is a major risk factor for epithelial defects and sloughing.16,31 EBMD is also considered a relative contraindication for LASIK; surface ablation being preferred in this situation. Other risk factors for epithelial defects include older age, skin type, thicker corneas and diabetes.35,36 In a prospective cohort study of 1852 eyes, 14% of patients experienced epithelial problems associated with their LASIK.37 Patients with pale skin that burns easily and patients with facial skin wrinkling had a 10 times greater risk of an epithelial defect. The risk of an epithelial defect was six times greater in patients over the age of 40 years and three times greater in patients with lighter hair or eye color. Interestingly, there was no relationship between Schirmer score and epithelial defects. An association was found between microkeratome features and epithelial defects, with certain keratomes and thicker flaps being associated with an increased risk. Nevertheless, patients with no previous signs or symptoms of EBMD may be at risk for large epithelial defects or sloughing even with better-designed microkeratomes that cause less compression during the creation of the flap. A simple test to determine epithelial adhesion prior to LASIK is to rub a cotton swab over the anesthetized ocular surface. If there is movement of the epithelium over the underlying corneal stroma, the epithelial adhesion complex is weak and the patient is at risk for developing an abrasion during the microkeratome pass. These patients are generally better candidates for surface ablation.
Management of Corneal Erosions
Most studies have failed to document an increased incidence of recurrent erosions following LASIK. However, in a postoperative questionnaire survey mailed to LASIK and PRK patients conducted by John A. Hovanesian, M.D., et. al., and responded to by 231 PRK patients and 550 LASIK patients, 8.0% of LASIK patients reported symptoms of recurrent erosion compared to 20.4 % of PRK patients.38 Patient satisfaction was highly associated with the absence of erosion symptoms.
Most LASIK surgeons insert a bandage contact lens in an eye that has experienced a significant epithelial defect at the time of surgery. The bandage contact lens serves two functions. It decreases postoperative pain and stabilizes the lamellar flap to help prevent flap dislocation and folds. The loss of the barrier function of the epithelium decreases flap adherence. For large epithelial defects, a small phototherapeutic keratectomy has been advocated to help promote epithelial reattachment.39
Limiting Issues, Maximizing Results
An understanding of the etiology of dry eye and the relationship between corneal erosions and LASIK will enable the refractive surgeon to take appropriate steps to minimize potential complications secondary to dysfunctional tear syndrome and corneal erosions. Knowledge of potential dry eye and the etiology of erosions will allow the surgeon to learn ways to maximize the stability of the ocular surface, minimize pre and postoperative complications and optimize the refractive outcome.
Renée Solomon, M.D., is a fellow working at Ophthalmic Consultants of Long Island, Rockville Centre office, and Eric Donnenfeld, M.D., is a partner of Ophthalmic Consultants of Long Island.
References
1. Kanellopoulos AJ, Pallikaris IG, Donnenfeld ED, et al. Comparison of corneal sensation following photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 1997;23:34-8
2. Linna TU, Vesaluoma MH, Perez-Santonja JJ, et al. Effect of myopic LASIK on corneal sensitivity and morphology of subbasal nerves. Invest Ophthalmol Vis Sci 2000;41:393-7
3. Chuck RS, Quiros PA, Perez AC, McDonnell PJ. Corneal sensation after laser in situ keratomileusis. J Cataract Refract Surg. 2000;26:337-9
4. Albietz JM, Lenton LM, McLennan SG. Effect of laser in situ keratomileusis for hyperopia on tear film and ocular surface. J Refract Surg. 2002;18:113-23
5. Pflugfelder SC, Jones D, Ji Z, et al. Altered cytokine balance in the tear fluid and conjunctiva of patients with Sjögren's syndrome keratoconjunctivitis sicca. Curr Eye Res. 1999;19:201-11
6. Afonso AA, Sobrin L, Monroy DC, et al. Tear fluid gelatinase B activity correlates with IL-1alpha concentration and fluorescein clearance in ocular rosacea. Invest Ophthalmol Vis Sci. 1999;40:2506-12
7. Prabhasawat P, Tseng SC. Frequent association of delayed tear clearance in ocular irritation. Br J Ophthalmol. 1998;82:666-75
8. Stern ME, Beuerman RW, Fox RI, et al. The pathology of dry eye: the interaction between the ocular surface and lacrimal glands. Cornea. 1998;17:584-9
9. Afonso AA, Monroy D, Stern M, et al. Correlation of tear fluorescein clearance and Schirmer test scores with ocular irritation symptoms. Ophthalmology. 1999;106:803-10
10. Wilson SE. Laser in situ keratomileusis – induced (presumed) neurotrophic epitheliopathy. Ophthalmology. 2001;108:1082-7
11. Sullivan BD, Cermak JM, Sullivan RM, et al. Correlations between nutrient intake and the polar lipid profiles of meibomian gland secretions in women with Sj�gren's syndrome. Adv Exp Med Biol. 2002;506 (Pt A):441-7
12. Kotani N, Hashimoto H, Kushikata T, et al. Intraoperative prostaglandin E1 improves antimicrobial inflammatory responses in alveolar immune cells. Crit Care Med. 2001;29:1943-9
13. Narumiya S, Sugimoto Y, Ushikubi F, et al. Prostanoid receptors: structures, properties, and functions. Physiol Rev. 1999;79:1193-226
14. Pholpramool C. Secretory effect of prostaglandins on the rabbit lacrimal gland in vivo. Prostaglandins Med. 1979;3:185-192
15. Gilbard JP, Rossi SR, Heyda KG, Dartt DA. Stimulation of tear secretion by topical agents that increase cyclic nucleotide levels. Invest Ophthalmol Vis Sci. 1990;31:1381-8
16. Ambrosio R Jr, Wilson SE. LASIK complications: etiology, prevention, and treatment. J Refract Surg. 2001;17:350-79
17. Gipson IK, Spurr-Michaud SJ, Tisdale AS: Anchoring fibrils from a complex network in human and rabbit cornea. Invest Ophthalmol Vis Sci. 1987;28:212-20
18. Zagon IS, Sassani JW, Ruth TB, McLaughlin PJ. Epithelial adhesion complexes and organ culture of the human cornea. Brain Res. 2001;11:205-13
19. Espana EM, Grueterich M, Mateo A, et al. Cleavage of corneal basement membrane components by ethanol exposure in laser-assisted subepithelial keratectomy. J Cataract Refract Surg. 2003;29:1192-7
20. Nishida T: Basic science: cornea, in Krachmer JH, Mannis MJ, Holland EJ, Palay DA (eds): Cornea: text and color atlas CD ROM. St Louis,MO, Mosby, 1998
21. Fogle JA, Kenyon KR, Stark WJ, Green WR. Defective epithelial adhesion in anterior corneal dystrophies. Am J Ophthalmol. 1975;79: 925-40
22. Azar DT, Spurr-Michaud SJ, Tisdale AS, Gipson IK. Altered epithelial-basement membrane interactions in diabetic corneas. Arch Ophthalmol. 1992;110:537-40
23. Laibson PR: Epithelial Basement Membrane Dystrophy, in: Krachmer JH, Mannis MJ, Holland EJ. Palay DA, (eds) Cornea: Text and Color Atlas CD ROM. St Louis Missouri, Mosby, 1998
24. Ambrosio R Jr, Possin D, Hong J, Wilson SE. Morphology of corneal epithelium in eyes epithelial slough during LASIK. ARVO abstract 2003, #3840.
25. Heyworth P, Morlet N, Rayner S, et al. Natural history of recurrent erosion syndrome�a 4-year review of 117 patients. Br J Ophthalmol. 1998; 82:26-8
26. Davidorf JM, Zaldivar R, Oscherow S. Results and complications of laser in situ keratomileusis by experienced surgeons. J Refract Surg. 1998;14:114-22
27. Shah MN, Misra M, Wihelmus KR, Koch DD. Diffuse lamellar keratitis associated with epithelial defects after LASIK. J Cataract Refract Surg. 2000 26:1312-18
28. Haw WW, Manche EE. Late onset diffuse lamellar keratitis associated with an epithelial defect in six eyes. J Refract Surg. 2000; 16:744-48
29. Dastgheib KA, Clinch TE, Manche EE, et al. Sloughing of corneal epithelium and wound healing complications associated with laser in situ keratomileusis in patients with epithelial basement membrane dystrophy. Am J Ophthalmol. 2000;130:297-303
30. Wang M, Maloney RK. Epithelial ingrowth after laser in situ keratomileusis. Am J Ophthalmol. 2000;129: 746-51
31. Updegraff S. Reactive epithelium syndrome. ARVO 2003, Abstract #2648
32. Castillo A, Diaz-Valle D,Gutierrez AR, et al. Peripheral melt of flap after laser in situ keratomileusis. J Refract Surg. 1998;14:61-3
33. Oliva MS. Ambr�sio Jr.R, Wilson SE. Influence of intraoperative epithelial defects on outcomes in LASIK for myopia. Am J Ophthalmol. In Press
34. Hsu JK, Johnston WT, Read RW, et al. Histopathology of corneal melting associated with diclofenac use after refractive surgery. J Cataract Refract Surg. 2003; 29:250-56
35. Tekwani NH, Huang D. Risk factors for intraoperative epithelial defects in laser in-situ keratomileusis. Am J Ophthalmol. 2002;134:311-16
36. Fraunfelder FW, Rich L. Laser-assisted in situ keratomileusis complication in diabetes mellitus. Cornea. 2002;21:246-48
37. Bashour M. Risk factors for epithelial erosions in laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:1780-88
38. Hovanesian JA, et.al. Symptoms of dry eye and recurrent erosion syndrome after refractive surgery. J Cataract Refract Surg. 2001;27:577-84
39. Kanellopoulos AJ, Perry HD, Donnenfeld ED. Intraoperative phototherapeutic keratectomy (PTK) in the management of microtome-related corneal abrasions (ICN) during LASIK. American Academy of Ophthalmology Final Program 2000;144:111.









