Looking
at SLT as a
Viable Option
SLT improves both patient quality of life and practice revenues.
MONTE
S. DIRKS, MD
In the 18 months since I started performing selective laser trabeculoplasty (SLT), it has become increasingly clear that this procedure is a safe and effective alternative to medication for glaucoma patients, maximizes the quality of my surgical time, and is a revenue-generating procedure for our practice.
In this article I will discuss clinical considerations for choosing SLT, practical logistics such as scheduling and staffing, and financial considerations when integrating this new procedure into a real-world practice.
|
|
|
|
ILLUSTRATION:
MARK ERICKSON/JIREH DESIGN
|
|
Patient Selection
Patients with angle-closure glaucoma, active neovascularization or active uveitis are not good candidates for SLT. Otherwise, SLT is a good option at any point in the therapeutic algorithm.
In my experience, people with heavy pigmentation, pseudoexfoliation, and pigmentary glaucoma do well after SLT. I like to use SLT as a primary therapy, giving patients the option of laser when we first make the decision they should be treated.
The important thing about SLT is that, rather than just being an additive to medications, it can replace medications. SLT allows you to help the patient maintain a stable IOP while replacing one or more expensive out-of-pocket medications with a procedure that is paid for by third-party insurers.
Patient Education and Marketing
Many patients have what I call "laser angst." Almost all of our geriatric patients have a family member or friend who has been treated with thermal laser for macular degeneration or diabetic retinopathy, usually with poor visual outcomes. As soon as we mention the word "laser," it triggers their fear of a similarly bad outcome. We have been able to reduce patient anxiety by referring to SLT as "cold laser" and explaining that it is entirely different from other laser treatments they may have heard about.
Internal marketing is important for successful integration of SLT. We educate all our glaucoma patients about SLT through posters, handouts and a short video that plays on a continuous loop in the waiting room. Moreover, our technicians are knowledgeable about the procedure, can discuss it with patients and immediately start looking at whether a patient is a candidate. Ultimately, however, the physician is the one who helps the patient make the decision. If you as a physician believe in the procedure, have excellent results, and can communicate those results, you will have a very high rate of conversion to SLT.
In office visits with glaucoma patients who are controlled on medication, I try to get a sense of their compliance in as non-threatening a way as possible. It is not at all difficult to tap into the underlying current of dissatisfaction that most patients feel with their glaucoma drops, which transitions nicely into an explanation of laser as an alternative.
External marketing is also critical. Advertising is a good way to get the word out, but news coverage is even better. Fortunately, we were able to get several TV and print news spots after pitching to the media that South Dakota was the first place between Denver and Minneapolis to offer the cold laser for glaucoma treatment.
Finally, happy patients provide the best external marketing. They generate buzz, or as I like to call it, "community conversation." This has led to more referrals than any other marketing we have done.
|
|
|
|
Table 1. The impact on my practice of converting a typical visit to check IOP on a medically-controlled patient to a same-day bilateral SLT. |
|
|
|
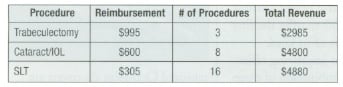
| Table 2: Comparative surgical reimbursement for a 2-hour O.R. slot. | |

|
|
| Table 3: Revenue impact of SLT on my surgical and total billings. |
Practice Considerations
As with any new procedure, the success of SLT in your practice depends partly on getting the logistics right. There are three basic ways to schedule SLT procedures: one at a time, for same-day opportunities; a few procedures before your regular clinic day; and large block scheduling. We have employed all three.
In South Dakota, where many patients travel long distances, it is important to me to be able to see a patient, and, if we decide to do SLT, do it the same day. Set-up and shut-down each takes about 5 minutes, and the procedure itself is relatively short, so a same-day procedure takes about 10 minutes of my technician's time and 5 minutes of mine. This is well worth the relatively short amount of time it takes to create a happy patient who can go home having been treated right away.
Initially, before there were many cases, my technicians would set up, counsel a couple patients and get the consent forms signed while I was at lunch. I would step in and do two procedures after lunch, before starting my afternoon clinic hours. I now find it most efficient to schedule many people in a block. I can comfortably treat six to eight patients in an hour, so in a typical 3 hour afternoon clinic I treat 18 to 20 SLT patients.
On SLT clinic days I have just two technicians assisting me. The pre op tech does counseling, the informed consent, and instills brimonidine. In the treatment room, I have an operative assistant who anesthetizes the eye, gets the Latina lens ready for me, cleans the lens after the procedure, and prepares the room for the next patient.
I choose to treat each patient 180� at a time per eye and have seen very positive results in the time we have utilized SLT in our practice. The response I have seen for retreatments is rather low, considering that volume for the total number of SLT treatments have just gone past the 1,600 mark recently.
In just 10% of patients, I have had to go back and treat the superior 180� for what I consider a "completion" rather than a retreatment.
The majority of patients who come back for this completion have a similar response as the initial treatment. In 80% of patients who have returned, we will see an additional 20% reduction in IOP with treatment of the superior 180�.
The Bottom Line
Currently, the average Medicare reimbursement in the United States for laser trabeculoplasty (Code 65855, either ALT or SLT) is $302 to $345, depending on whether the procedure is done in the office or in a facility.
The consulting fee is higher if you make the decision (properly documented) to do surgery. My Medicare procedure fee is $305 per eye. I often treat both eyes at the same visit, with just one follow-up visit, which is outside the 10-day global period for SLT. As you can see, the decision to do SLT increases revenues by a factor of 10, from $60 to $675, for that one patient.
SLT is also an efficient use of your surgical time. On some days, I get the OR for 2 hours after my cataract partner is done. In that time, I can do just three trabeculectomies. From a revenue perspective, it is far more beneficial to the practice to do cataract surgery or SLT in those 2 hours (Table 2).
It makes sense for the practice to maximize your surgical time. But even more important is maximizing the impact you have on your patients. In those 2 hours, I could help 16 patients get off medications, or I could start three patients on the rather long, complicated post-trabeculectomy course. That is not a tough choice.
Finally, it is important to look at the return on investment for the practice. When I first presented the idea of buying this laser to my partners in March 2003, they scoffed at the idea of buying a $60,000 laser that "only did one thing." But I was convinced that SLT would be good for our patients, so I borrowed the $60,000 on my own. I figured I needed to do at least 100 SLT cases per year (more than double the number of ALT cases I had done previously) to break even. I rapidly surpassed the break-even point, and now do as many as 100 SLT cases per month, so cash flow has not been a problem.
The population of Rapid City is only 70,000, but we draw patients from a 300-mile radius. I have about 3,000 glaucoma patients who generate about 10,000 visits yearly — numbers that I think are typical of a glaucoma practice.
I am a bit uncomfortable focusing on the financial aspects of this technology because I think our primary goal as doctors is to serve our patients the best way possible. But I do think it is important for glaucoma specialists to understand that performing SLT will have a positive impact both on patients and on the bottom line.
I think selective laser trabeculoplasty is going to be the new standard of care for glaucoma. It allows us to offer patients a safe and effective alternative to drops and their accompanying quality-of-life and compliance problems. It has had a tremendous impact on patient satisfaction in our practice, and has also brought a nice improvement to our bottom line.
Monte Dirks, M.D., is in private practice at Black Hills Regional Eye Institute in Rapid City, S.D. He can be contacted at (605) 341-2000.