AMD: A
Changing Diagnostic and Management Paradigm
A new detection device and research findings
are
empowering general ophthalmologists to treat
AMD patients.
BY
JOHN PARKINSON, ASSOCIATE EDITOR
According to amd.org's Web site, as many as 14% to 24% of United States' population aged 65 to 74 and 35% of people aged 75 or older presently have the disease. Compound this with the eldest group of baby boomers turning 60 this year, and millions more to follow in the years to come, and ophthalmologists can see the potential proportions of AMD.
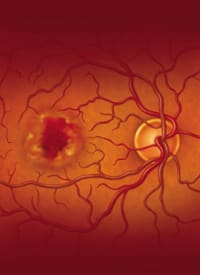
Traditionally, diagnostic and treatment options have been limited for all AMD patients. More recently, general ophthalmologists who see AMD patients that have not yet progressed to choroidal neovascularization (CNV) possess more technology and research information to not only help detect CNV but to manage the disease before it progresses to advanced stages.
In light of these changes, this story will detail how some doctors are managing AMD patients who are at risk of developing advanced dry or wet AMD.
New Detection Technology
One diagnostic instrument that is being studied and used in practices is the PreView Preferential Hyperacuity Perimeter (PHP) from Carl Zeiss Meditec. For general ophthalmologists who see AMD patients, the Preview PHP can be viewed as early detection technology for monitoring dry AMD patients' possible progression to CNV.
While fluorescein angiograms continue to be viewed as the gold standard for diagnosis, they are not used as monitoring procedures due to their invasive nature, cost and side effects.
Neil Bressler, M.D., James P. Gills professor of ophthalmology in the Wilmer Eye Institute at the Johns Hopkins University School of Medicine, presented results of an international, multi-center clinical study. Sixty five patients with confirmed onset of CNV and 57 patients with intermediate dry AMD were tested with the PHP. The results showed the PHP had a sensitivity of 82% in detecting CNV and a specificity of 88% in differentiating dry from wet AMD.1
The PHP is a non-invasive perimetry test set up to measure patients' abilities to detect distortion in the central visual field. When administering the test, patients sit in front of a computer monitor that presents a series of linear dot patterns to the central 14Þ of the visual field. Each pattern includes an artificial distortion of varying magnitudes. Patients must determine what they perceive as the location of the most prominent distortions. The test's simulation of distortion and the patient's visual distortion from the effects of AMD serve as competing stimuli that determine the relative depth and location of the patients' visual field defect.
Patients are instructed to touch the location on the monitor where the distortion is most prominent. The response patterns are recorded and automatically analyzed by a customized algorithm, and the PHP compares the responses to a normative database. The PHP then generates a map that identifies visual field defects and provides confidence and reliability parameters. The reliability parameters give the operator the degree of false positive and false negative errors. The confidence parameters provide the operator with the likelihood the patient's test results are consistent with CNV or intermediate AMD.
Conversions to CNV
Two general ophthalmologists who use the PreView PHP have shared their conversion data with Ophthalmology Management. Sara Sirkin, M.D., has tested 62 patients with the PHP thus far. There has been 1 confirmed conversion to CNV; 2 probable conversions; 1 false positive for CNV; and 1 whose conversion was a probable visual defect caused by geographic atrophy.
Dr. Sirkin breaks down the test results. "The first patient has been confirmed by OCT and FA and is now in treatment," explains Dr Sirkin. "The [one probable] was complaining. The PHP showed probable progression, the OCT showed elevation, the FA showed questionable leakage and is now being followed. The second [probable] patient showed a defect on PHP, OCT and clinical exam. [This patient] has been sent to retinal specialist, but I do not yet have the follow-up. The patient who was a false positive, showed conversion on the PHP and OCT, but the FA did not show any active leakage. The last patient had a PHP conversion, but the OCT showed atrophic macula and she was not sent on to a retinal specialist."
Walter Fried, Ph.D., M.D., has tested 55 patients. Two patients tested positive for CNV progression on the PHP; their results were confirmed with an FA. It is notable that several physicians have reported similar, positive CNV test results that were verified in the OCT exam, but the FA did not show active leakage. In at least two of these cases, the patient returned for a second PHP test several months later and after having a second positive PHP test showing an even larger visual field defect, the patient was sent for a second FA, which then showed distinct CNV leakage.
Monitoring Strategies and Co-Management
Dr. Sirkin uses the PHP in her practice for intermediate dry AMD patients and for those who have lost vision in one eye due to wet AMD. "Most of the dry AMD patients we are seeing every 6 months, and so every time they come in we'll do the PHP," explains Dr. Sirkin. "If the initial PHP has shown a suspicious spot and there is no other evidence and the patient is not having any complaints, I probably will start to see [the patient] every 4 months."
Contrary to those type of patient situations, if Dr. Sirkin is following a patient who has some vague complaints but she does not see anything clinically or they have not already been tested with the Preview PHP, she will order a test. If testing shows progression of AMD, the patient is given an OCT exam; if that shows signs of macular edema or CNV, she will refer that patient to a retina specialist.
From a clinical standpoint, Dr. Sirkin sees the adoption of such technology as furthering patient monitoring. "I always look closely at my macular degeneration patients, but I think it [PHP] is making me look at them closer," she says.
|
|
|
|
The Preview PHP is a non-invasive perimetry
test designed to detect the onset of CNV and can be easily utilized by technicians. |
One of the diagnostic tools to which PHP has been compared is the Amsler Grid. In a recent study, PHP was found to be twice as sensitive as the Amsler Grid in detecting AMD-related lesions. However, there was a relatively high rate of false-positive results (18%) for healthy individuals with the PHP. The study's authors did note some limitations to the study such as the different color backgrounds used for the Amsler and PHP.2
While the Amsler Grid is usually given to patients to use at home, the PHP is used strictly in doctors' practices. Doctors are still asking patients to test themselves with the Amsler Grid, but they know its limitations. Retina specialist Nalin Mehta, M.D., uses both the Amsler and the PHP and points to the greater sensitivity of the latter to pick up abnormalities. "There is a 'glass ceiling' of sensitivity that you reach with the Amsler Grid; with the PHP you break through this glass ceiling."
Dr. Fried discusses the "unpleasant experience" of having a patient go from a contained dry early stage in one visit to developing a hemorrhage in the interim of the next visit. And even though Dr. Fried had the patient on Amsler Grid testing at home, the patient still came in earlier than the next scheduled appointment complaining of vision loss.
"With the PreView PHP, I'm able to monitor for early distortions consistent with wet AMD. So if something funny shows up, I can then send a patient off to the retina specialist before the damage becomes symptomatic," says Dr. Fried.
For Dr. Fried's patients who show signs of dry AMD but have not progressed to advanced in wet or dry forms, he will see them three times a year, performing a PHP test for two of the visits consecutively and he will then perform a comprehensive macula exam on the third visit.
For general ophthalmologists who see AMD patients, a co-management relationship may arise with retina specialists where each doctor will care for the patients according to his or her own medical specialty. Dr. Fried has a retina specialist who leases office space in his practice, so he can conveniently refer advanced or wet AMD patients in-house. "He's [the retina specialist] in my office, so if I find anything I think he needs to see, I just refer to him," says Dr. Fried. "He then takes care of it, and he will follow the patients as long as he thinks it is appropriate. He will send them back to me for refractions, cataracts, treatment of glaucoma and anything else that shows up when he is taking care of them."
While retinal specialist, Joe Murphy, M.D., doesn't have a PHP in his practice, he sees patients who are referred to him by general ophthalmologists in his area (Buffalo, N.Y.) that do possess the technology. In these types of situations — when a local general ophthalmologist sees an abnormality in a PHP test and the patient is referred to Dr. Murphy — he will confirm a wet AMD diagnosis.
Dr. Murphy stresses the importance of being able to diagnose CNV as early as possible, because patients who are diagnosed in later stages of CNV have less treatment options available to them.
"It's like breast cancer; early detection is the key," explains Dr. Murphy. "The value of this tool [PHP] is if you catch the disease early while lesions are small. Those lesions respond better, and ultimately, you can preserve more vision."
Dr. Mehta also views early detection as paramount, especially after witnessing the ravages of AMD progression and the resulting deterioration of a patient's sight. While he is still in the process of refining a final algorithm for exactly when and how often he will utilize PHP testing, he weighs his decision to use the PHP based on clinical exams, his intuition and whether the patient is a good candidate for nutritional supplements.
Dr. Mehta uses the National Eye Institute's Age-Related Eye Disease Study (AREDS) guidelines as a qualifier for PHP testing. "If patients meet the criteria for vitamins under the AREDS study utilizing the definition for intermediate macular degeneration, I would generally consider initiating PHP testing 2 to 4 times a year."

The subject of nutrition affords general ophthalmologists the opportunity to educate their patients and give AMD sufferers some autonomy in managing their disease. Many ophthalmologists are familiar with the aforementioned AREDS trial; the ongoing research testing the effectiveness of specific vitamins and minerals on the incidence and progression of AMD.
Another AREDS study entitled, AREDS II, will be conducted in the future. AREDS II will evaluate the efficacy of lutein (10 mg) plus zeaxanthin (2mg) together and/or omega-3 long-chain polyunsaturated fatty acids plus eicosapentaenoic acid at a total of 1 g in decreasing the risk of progression to advanced AMD compared to a placebo.3 NEI is looking at the lutein/zeaxanthin relationship and the appropriate ratio the two carotenoids should be ingested.
Elizabeth Johnson, Ph.D., scientist at the Carotenoids and Health Laboratory at the Jean Mayer US Department of Agriculture Human Nutrition Research Center on Aging at Tufts University, has performed research on the relationship of AMD with lutein and offers some insight into the carotenoid.
"Because of what we know about lutein and AMD, it is one of the most compelling nutrients/disease relationships that I can think of," says Dr. Johnson. "Lutein is a yellow pigment, and being yellow the specifics of that means it's going to absorb blue light."
Dr. Johnson goes on to explain that not only does lutein protect against harmful light, but it also acts as an antioxidant against the oxidative stress in the eye. Along with those two protective qualities, there is a 1,000 times greater concentration of lutein in the macula than anywhere else in the body. Therefore, the nutrient should not be overlooked when looking at a patient's nutritional intake.
She says the 6 to 10 mg of lutein that fellow researchers are debating as useful in the fight against AMD are not harmful to most people, so she does not see a problem in ophthalmologists talking to their early and intermediate AMD patients about increasing their intake to a 6 to 10 mg daily allowance. Dr. Johnson points out that while most Americans only average about 1 to 2 mg of lutein, it is quite easy to get the recommended daily allowance by eating a cup of spinach daily. The exceptions for this type of food recommendation are for patients who might be prone to kidney stones or those on blood thinning drugs. For these patients, Dr. Johnson recommends an oral supplement.
Statins and the Vascular Model
A short-term study published last year showed evidence that taking statins and aspirin were associated with decreased rates of CNV among AMD patients.4
One of the study's investigators, Jacque Duncan M.D., assistant professor of ophthalmology at the University of California, San Francisco, discusses the limitations of this and all studies done to date.
"The data supporting a relationship between statin use and reduced risk of AMD so far have come from retrospective and cross-sectional studies. In general, data from these types of studies are more likely to reflect bias than studies done prospectively," says Dr. Duncan. "The prospective cohort data so far have not shown a convincing relationship, so I think it is still premature to prescribe statins purely for the purpose of reducing risk of AMD or AMD progression."
Nonetheless, Dr. Duncan thinks longer follow-up of existing studies may someday reveal an association between statins and lower AMD progression. Until then, Dr. Duncan is only recommending statins to patients with elevated cholesterol or other medical reasons aside from AMD.
Conversely, Ephraim Friedman, M.D., professor of ophthalmology at Harvard Medical School, is an advocate for prescribing statins for all patients with AMD. "I advocate the use of statins at any stage or [for any] type of AMD, states Dr. Friedman. "I do so because I think the statin will affect the deposition of lipids in the eye, a step in all forms of AMD."
Dr. Friedman's reference about statins affecting the lipid deposits in the eye comes from his research on what he refers to as "the vascular model of AMD." He, along with other researchers, developed this model after finding evidence that AMD shared epidemiologic risk factors and pathogentic mechanisms with angiosclerosis.5
Specifically, the model's hypothesis holds that AMD is a vascular disorder that is characterized by impairment of choroidal perfusion of the retinal pigment epithelium, and that lipids accumulate in drusen and in Bruch's membrane because the choriocapillaris does not clear them.6
So along with statin research, Dr. Friedman is including antihypertensives into his studies. While being a proponent of statin therapy, Dr. Friedman does point out that some patients respond negatively and severely to statins, but this is a small group of people, relative to the numerous amount of people who could benefit from statin therapy.
General Ophthalmologist's Role
With the news that statins may affect the progression of AMD, general ophthalmologists are looking into the possibility of including a drug regimen to a patient's treatment. Along with recommending his patients take AREDS supplements, and eat green leafy and yellow vegetables, Dr. Fried also considers the addition of a statin.
"I will check to see if they are on it; I will talk to them about their cholesterol, and target their nutrition to lower their fats," says Dr. Fried. If that patient is not on a statin medication, Dr. Fried will communicate with the patient's primary-care physician by sending a letter discussing the possibility of adapting a pharmacological regimen. Dr. Fried will explain to the doctor that statistically � but not in a double-bind study �there is a lower incidence of AMD among people who take statins.
�I�m not sure if the evidence is there to put somebody with low cholesterol on a statin at this point. It may simply mean that low cholesterol is what helps people with macular degeneration not the statin. I suspect that people on the statins probably have somewhat lower cholesterol than normal people,� points out Dr. Fried.
Dr. Fried says researchers have not confirmed if it is the ability to lower cholesterol, the anti-inflammatory component of the statins or both that are helpful. Nonetheless, if one of his patients is a borderline candidate for a statin, he will recommend it to the primary-care physician.
As general ophthalmologists have a diagnostic instrument to help in detecting the onset of CNV, the ability to educate patients on the benefits of nutritional supplements and the potential of statins and other oral pharmacological treatments, their roles as the first line of defense in AMD detection and management have increased substantially. With her AMD patients in mind, Dr. Sirkin remains vigilant for any continuing research findings and developing technological diagnostics. �Since general ophthalmologists are still the gatekeepers, so to speak, we have to be really aware of what�s going on.�
Footnotes
1. Bressler N. Preferential
Hyperacuity Perimeter for detecting choroidal neovascularization study.
Presented at the American Academy of Ophthalmology Meeting; New Orleans, LA,
2004.
2. Preferential Hyperacuity Perimeter Research Group. Results of a multicenter
clinical trail to evaluate the preferential hyperacuity perimeter for detection
of age-related macular degeneration. Retina. 2005; 25: 296-303
3. Chew EY. Dietary supplements: what we should and should not be recommending
for our patients. Retinal Physician. 2005; 2:45-47.
4. Wilson HL, et al. Statin and aspirin therapy are associated with decreased
rates of choroidal neovascularization among patients with age-related macular
degeneration. American Journal of Ophthalmology. 2004; 137: 615-24.
5. Friedman E, et al. The relationship of statin use to the development of AMD.
Poster presented at the Association for Research in Vision and Ophthalmology
meeting; Ft. Lauderdale, FL, 2005.
6. Friedman E. Update of the vascular model of AMD. British Journal of
Ophthalmology. 2004; 88:161-63.









