Glaucoma Case Studies
Case One: Tissue Plasminogen Activator after Trabeculectomy
BY SONAL D. WADHWA, M.D., DAVID CHIA, M.D., AND EVE J. HIGGINBOTHAM, M.D.

The management of filtering blebs after trabeculectomy can sometimes have a rocky course. An uncommon but treatable cause of bleb failure can be blood in the sclerostomy site blocking flow of aqueous through the scleral flap. Here, we present a case where intracameral tissue plasminogen activator (tPA) quickly resolved this postoperative complication, which if left untreated could have easily resulted in bleb failure.
Case history/presentation: A 62-year-old African American female with primary open-angle glaucoma on maximal tolerated medical therapy was not meeting the target intraocular pressure (IOP) in her right eye. Her visual acuity in the right eye was 20/70 and IOP was 20 mmHg. Her past medical history was significant for diabetes and hypertension, and she was on daily aspirin therapy.
Treatment: The patient underwent uncomplicated limbal-based trabeculectomy in the right eye with mitomycin C applied for 2.5 minutes. Post-op day 1, her vision was 20/400 and IOP was 2 mmHg. Slit lamp exam revealed a deep anterior chamber (> 3 central corneal thicknesses) and a diffuse, low-lying, seidel-negative bleb. At this time, she was started on prednisolone acetate 1% q2h, atropine sulfate 1% bid, and neomycin/polymyxin B and dexamethasone ophthalmic ointment (Maxitrol) qhs.
On post-op day 5, her vision was counting fingers at 5 feet, and IOP was 8 mmHg. There was a new 5% hyphema in the anterior chamber. The anterior chamber was deep and the bleb was unchanged. The patient was instructed to stop taking her daily aspirin.
On post-op day 8, her vision was 20/80 and IOP was 36 mmHg. Slit lamp examination showed resolution of the hyphema and a flat, vascularized bleb. Gonioscopy revealed a blood clot in the sclerostomy site.
At this time, digital massage was performed without improvement in IOP or bleb elevation. Argon laser suture lysis was performed to cut one suture, and IOP dropped to 28 mmHg. The patient was started on dorzolamide 2% and timolol 0.5% (Cosopt) OD bid as a temporizing measure while tPA was obtained for intracameral injection.


On post-op day 9, visual acuity was 20/80 and IOP was 26 mmHg. The bleb was flat and there was still a clot within the sclerostomy site. TPA was administered intracamerally 10 mcg/0.1 cc for a total of 0.25 cc (25 mcg). Ten minutes after injection the IOP was 10 mmHg.
Discussion: Blood in the sclerostomy flap is uncommon after filtering surgery, but can quickly lead to bleb failure if not treated promptly. First, conservative management should be initiated to try to dislodge the clot. Sometimes digital massage by the physician can prove to be enough to displace the clot. Argon suture lysis can also be performed, as it allows more aqueous flow to dislodge the blood clot. When those measures fail, the use of intracameral tPA can be very useful as demonstrated in the above case.
TPA is a type of thrombolytic drug. Other drugs in this class are streptokinase and urokinase. TPA is a naturally occurring protease enzyme found in humans. It was first isolated in human melanoma cells, but now is manufactured for therapeutic purposes by using recombinant DNA. TPA is involved in the fibronolytic system, which is responsible for clot dissolution. It activates the conversion of plasminogen to plasmin. Plasmin, one of the main fibrinolytic enzymes, degrades fibrin, which is a protein that maintains the structural integrity of blood clots.
TPA is commonly used in the management of acute myocardial infarction to dissolve clots in the coronary circulation. It has recently been used, though with some controversy, in the management of acute ischemic strokes by neurologists. In ophthalmology, tPA has been used as an intravitreal injection by retina specialists to treat submacular hemorrhages secondary to age-related macular degeneration. TPA has also been reported to aid the treatment of excessive fibrin after cataract extraction or vitrectomy surgery. Glaucoma specialists have used TPA intracamerally1 for cases like the one described here and also subconjuntivally2 for blood clots that arise in blebs. TPA has been used in dosages of 2 mcg to 25 mcg intracamerally or subconjunctivally for the treatment of post-trabeculectomy fibrin or blood clots. With the use of intracameral tPA, there is the risk of hemorrhage that can lead to rebleeding and hyphema. Therefore, although tPA does have some risks, it may often salvage a bleb that may otherwise fail.
Drs. Wadhwa, Chia and Higginbotham submitted this case from the University of Maryland Department of Ophthalmology and Visual Sciences.
REFERENCES FOR CASE ONE:
1. Lundy DC, Sidoti P, Winarko T, et al. Intracameral TPA after glaucoma surgery. Ophthalmology. 1996;103:274-282.
2. Ortiz JR, Walker SD, McManus PE, et al. Filtering bleb thrombolysis with TPA. American Journal of Ophthalmology. 1988;106:624-625.
Case Two: Optic Nerve Imaging Aids in Diagnosis
BY STANLEY J. BERKE, M.D., F.A.C.S.
Case history/presentation: A 37-year-old African American female was referred to us for evaluation as a glaucoma suspect. Previous examinations had found an IOP of 22 mmHg OU with "normal" optic nerves and a superior nasal field defect OD. Her family history was negative for glaucoma. She didn't have any systemic diseases and wasn't taking any medication.
Examination: My exam found:
► The patient's uncorrected vision was 20/20 OU; as in the previous exams, her IOP was 22 mmHg OU.
► Pachymetry revealed slightly thin central corneas (525 microns) OU.
► Her anterior segment examination, gonioscopy and funduscopic examination were normal.
► Her optic nerves and stereoscopic disc photographs appeared normal, with cupping OD 0.4 x 0.4 and OS 0.3 x 0.3 (see images on next page).
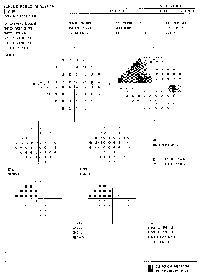
► Visual fields, which were normal OS, showed a superior nasal step OD (see visual fields on next page).
Because of the visual field finding, I performed HRT II scans (see results on next page). The scans showed significant cupping to the inferotemporal rim OD, corresponding to the superior nasal visual field defect OD. The scan OS was normal, corresponding to the normal visual field test.
The results of the HRT II scan prompted me to re-evaluate the optic nerves. This time, I detected subtle sloping of the cup OD to the inferotemporal rim that I hadn't noticed during my initial evaluation and review of the stereo optic disc photos. As a result, I diagnosed primary open-angle glaucoma and initiated glaucoma treatment in the right eye. (I decided to continue to monitor the left eye without treatment.)

|

|

|
|
|
Before re-evaluation, the patient's optic nerves and stereoscopic disc photographs appeared normal. |
Visual fields were normal OS, but showed a superior nasal step OD. |
Discussion: This case demonstrates the immediate usefulness of the HRT II in evaluating a glaucoma suspect. In many of these cases, details of the configuration of optic nerve cupping aren't readily apparent, even with careful observation. The HRT II scan in this case quickly and accurately revealed the optic nerve pathology in the right eye and helped to establish an immediate diagnosis.
In addition to being a valuable tool for diagnosis, I've found the HRT II scans to be useful for patient education. They clearly show optic nerve abnormalities, which can then be correlated to visual fields. Education often improves compliance with follow-up exams and use of medication.

|

|
| HRT II scans showed significant cupping to the inferotemporal rim OD, corresponding to the superior nasal visual field defect OD, prompting re-evaluation of the optic nerve. The scan OS was normal, corresponding to the normal visual field test. | |
Dr. Berke is an associate professor of ophthalmology and visual sciences at Albert Einstein College of Medicine in New York. He is chief of glaucoma services at Nassau University Medical Center on Long Island, and is a founding partner of Ophthalmic Consultants of Long Island. He has no financial interest in the HRT II.








