The Five R's of Optic Nerve Examination
Evaluation
of the optic nerve can diagnose and assess existing primary open angle glaucoma.
RONALD L. GROSS, M.D.
It is important that we integrate optic nerve examination into our clinical practices. This will allow us to properly evaluate and document the optic nerve, assess the disease severity and set appropriate target pressures based on the patient's risk factors including the severity of glaucomatous damage to the optic nerve.
|
|
|
|
A
good method for obtaining the size of the optic disk is by using indirect ophthalmoscopy
lenses at the slit lamp.
|
|
By reaching target IOPs, we can decrease the risk of progression. However, re-evaluation of structure and function is critical to assess the efficacy of treatment. If progression is found, then it is necessary to reset and achieve lower target pressure to minimize the risk of further progression.
The 5 R's is a concept created by Robert N. Weinreb, M.D., Felipe Medeiros, M.D., and Remo Susanna, Jr., M.D., and can be utilized to standardize the examination and documentation of the optic nerve and nerve fiber layer. This will allow the clinician to assess the optic disc and nerve fiber layer with confidence in determining the presence and severity of glaucomatous damage.
This article will define the 5 R's, explain how doctors can use examination techniques in their practices and discuss IOP treatment.
Rule Number 1. The edge of the optic disk is the opening of the scleral canal and in most patients it is easily determined. Once the edge of the optic disk has been identified, it is important to measure the size of the optic disk. There are several methodologies that are available to accomplish this. The direct ophthalmoscope is the simplest to use, with the smallest white light aperture (5Þ). The size of this light spot with the patient's refractive correction in the direct ophthalmoscope represents approximately the size of the normal optic disk. When the light is superimposed over the disk, if the disk is substantially larger than the light, it represents a large disk. If it is substantially smaller, it most likely represents a small disk. A more quantitative way involves the use of indirect ophthalmoscopy lenses at the slit lamp. By adjusting the height of the slit, using the scale to coincide with the vertical or horizontal size of the disk, one can calculate the size of the disk. If a 60-diopter lens is used, the value on the scale directly represents the size of the disk. Using a 78-diopter lens, a conversion factor of 1.1 must be multiplied to the value on the scale to get the disk diameter. With a 90-diopter lens, use a conversion factor of 1.3. The average vertical disk diameter is approximately 1.8 mm. The average horizontal diameter is approximately 1.7 mm.
Measurement of the disk size is important because there is great variability in the size of the optic disk. One of the most common causes of a large optic cup is a large disk. Small disks tend to have a vertical diameter of less than 1.5 mm; large disks tend to have a vertical diameter of greater than 2.2 mm. Thus, in a disk that is small even a slight increase in size of the cup may have substantial implication; whereas, in a very large disk, a very large cup may be normal. Unfortunately there are some disks, such as the highly myopic disk, in which it is difficult to accurately assess this factor. However, in the vast majority of patients, these techniques are successful.
|
|
|
|
Close
examination for possible hemorrhages is significant as they are believed to be a
sign of disease progression. |
Rule Number 2: Doctors must identify the size of the neural retinal rim. This is the classic way focal glaucomatous damage has been assessed, by loss of the neural retinal rim. The rim is defined as the distance between the border of the disk and the edge of the cup. In most normal patients the width of this neural retinal rim follows the "ISNT" rule- that is the Inferior neuroretinal rim is the thickest, followed by the Superior, the Nasal with the Temporal neural rim being the thinnest. When there is focal loss of the neuroretinal rim — we refer to this as a notch — that may or may not extend all the way to the edge of the optic disk.
Glaucoma causes loss of the neural retinal rim; it does not cause pallor of the remaining neuroretinal rim. If the remaining neural rim is pale, this likely is not the result of glaucoma and the patient should be worked up for other causes of non-glaucomatous optic atrophy.
Rule number 3. The retinal nerve fiber layer represents the axons of the retinal ganglion cells that are coursing toward the optic nerve to exit the eye. These can actually be seen using red-free light, looking at the striations and the brightness of these fibers. The nerve fiber layer tends to be thickest superiorly and inferiorly and bright striations typically are there. Retinal nerve fiber layer loss may be diffuse in which case it is often difficult to identify. A subtle sign of this characteristic may be a sharpening of the edges of the retinal vessel as retinal nerve fiber layer is no longer covering them. Often, localized retinal nerve fiber layer loss is useful and coincides with an area of notching of the neural retinal rim although it may precede notching.
Rule Number 4. When examining the region of parapapillary atrophy, there are two types of atrophy to be aware of: the alpha zone containing both hypo- and hyper-pigmented areas, which may be present in normal eyes as well as glaucomatous eyes, and the beta zone that is more common in glaucomatous eyes.
This is atrophy of the retinal pigmentary epithelium and choriocappilaris leaving only large choroidal vessels visible. It has been shown that beta zone atrophy is present in the same area of the disc in which glaucomatous damage is present It has also been suggested that progression of the beta zone is associated with progressive glaucomatous loss.
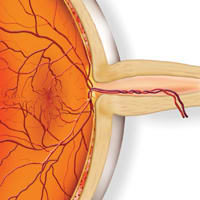
Rule Number 5. A suspicion of glaucoma progression is increased when a retinal and optic disk hemorrhage is found. These are typically flame-shaped hemorrhages in the nerve fiber layer on or adjacent to the edge of the disc. They are usually present for 1-3 months. It is important to carefully examine the optic disk as the disk hemorrhage may be quite subtle. If present, this hemorrhage has been shown to correlate with increased risk of glaucomatous damage. Strong consideration should be given to advancing therapy. Frequently, follow-up to assess a hemorrhage is appropriate.
|
The 5 R's |
|
Rule Number 1 observe the scleral ring to identify the limits and size of the optic disk. Rule Number 2 identify the size of the neural retinal rim. Rule Number 3 examine the retinal nerve fiber layer. Rule Number 4 examine the region of parapapillary atrophy. Rule Number 5 look for retinal and optic disk hemorrhage. |
|
Monitoring IOP
Intraocular pressure is still the primary factor in glaucoma management. There are population studies showing the incidence of severity and progression of glaucoma correlates with elevated intraocular pressure. Intraocular pressure reduction is the only current treatment modality for decreasing the risks of disease progression.
We are fortunate in that over the past several years numerous glaucoma clinical trials have been performed to provide data to guide us in intraocular pressure. These studies are relatively large, well-designed, well-performed studies looking at treatment versus observation, or comparing two modalities of treatment over long periods of time. In studies where treatment is compared to observation, the treated group always has a lower risk of progression than the untreated group.
In those studies comparing different modalities of treatment, those patients who were receiving the most aggressive treatment, either by the magnitude of pressure lowering or the consistency of pressure lowering, have the least risk of progression. The Collaborative Initial Glaucoma Treatment Study showed a 38% to 46% reduction in IOP, and on average there was no progression over 5 years.
Treatment for glaucoma should be initiated when there is evidence in the optic disk, nerve fiber layer or visual field that is characteristic of the disease. Often, by the time the visual field abnormality is detected, substantial optic nerve damage has occurred. Thus progressive damage to the optic disk and the retinal nerve fiber layer alone is sufficient for the diagnosis of glaucoma and the initiation of treatment.
Adding the 5R's
When using the 5R's examination technique, it needs to be combined with visual field and intraocular pressure data. Visual field testing is important as reproducible visual field defects confirm the presence of glaucoma. Visual fields are critical in patients with more advanced disease where the optic nerve change may not be easily recognized because of the severe damage present. By including the 5R's into one's examination regimen, doctors have a methodology for detecting and documenting glaucomatous damage.
Ronald L. Gross, M.D., is professor of ophthalmology at Baylor College of Medicine and the Cullen Eye Institute in Houston, Texas. He can be e-mailed at rgross@bcm.tmc.edu.