Glaucoma Case Studies
Case One: Low-tension glaucoma: diagnosis and management
Examination:
- Best-corrected visual acuity (BCVA) was 20/40 in both eyes
- No afferent pupillary defect was present
- Tonometry showed intraocular pressure (IOP) of 12 mmHg OU
- Anterior-segment exam was normal
- Gonioscopy reveled open angles bilaterally
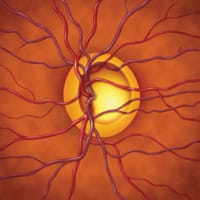
- Dilated-fundoscopic exam revealed advanced cupping of both optic nerves, with cup to disc ratios of 0.95 OU. Peripapillary atrophy was also recorded on the exam.
Treatment: The patient subsequently left the country, missing his scheduled follow-up appointment. Instead, he sought treatment in Shanghi. An Octopus visual field was performed and based on the results the patient was started on latanoprost (Xalatan) OU.
When the patient returned to the United States, he presented to our glaucoma clinic approximately 6 months after his initial exam. His BCVA was unchanged, his tonometry was 11 mm Hg OU, and gonioscopy showed both angles open to scleral spur OU. Pachymetry revealed corneal thicknesses of 518 microns in the right eye and 545 microns in the left eye. Optic-nerve examination correlated with the findings noted previously.

|
|
|
In these optic disc photos, severe cupping of the nerve and
peripapillary atrophy were noted. Images courtesy of Faris R. Ghosheh, M.D., and Eve J. Higginbotham, M.D. |
|
Our initial management was to obtain Humphrey visual fields (HVF) 24-2 OU and to start a latanoprost reverse monocular trial (i.e., stopping the medication OS). The HVFs 24-2 showed bilateral superior arcuate defects. The field was repeated 2 weeks later and the defects were reproducible.
The patient returned 1 month later. Intraocular pressure was 9 mmHg OD and 12 mm Hg OS. We recommended starting latanoprost OU based on the result of the monocular trial. We also obtained a HVF 10-2, which showed a small island of vision bilaterally. The HVF was repeated 2 weeks later and the defects were reproducible. Optic disc photos were also obtained. (See image above.)
Based on the previous findings, we initiated a work-up for low-tension glaucoma (LTG). We first obtained a diurnal curve to rule out possible pressure spikes occurring during the day. Intraocular pressures during the curve ranged from 8 mmHg to 12 mm Hg OU. The patient also underwent a magnetic resonance imaging of the brain, which was normal. His blood work for complete blood count, rheumatoid factor, erythrocyte sedimentation rate, anti-nuclear antibody, and syphilis was normal.
On subsequent follow-up, we obtained a Heidelberg retinal tomography (HRT), which confirmed advanced glaucoma OU. We also referred the patient for a sleep study because he was complaining of fatigue and restless sleep throughout the night. His primary care physician recently prescribed zolpidem (Ambien).
The sleep study revealed severe obstructive sleep apnea with prolonged periods of decreased oxygen saturation. He was started on Continuous Positive Airway Pressure (CPAP) and was reportedly sleeping better. Currently, he continues to use latanoprost OU. His subsequent HRT showed no progression of his glaucoma and we are following him closely.
Discussion: Low-tension glaucoma is a challenging and controversial diagnosis. Intense debate has surrounded LTG since it was proposed by von Graefe in 1857. One school of thought categorizes LTG as a distinct entity, having unique findings and rates of progression. However, others feel LTG is in the same continuum of primary open-angle glaucoma (POAG) and a separate category for LTG implies different etiologies that do not exist.1 We believe that LTG is a diagnosis of exclusion and when patients appear to be losing fields and optic-nerve head tissue with low pressure, a careful history and work-up is necessary to be sure other factors are not contributing.
In the examination of LTG patients, salient aspects of patient history to ask about are prior events that may have led to transient IOP spikes. For example, prolonged topical steroid use for inflammatory diseases or infections can result in short periods of high IOP, which can cause optic-nerve damage. Likewise, it is important to ask about past ocular surgeries because postoperative pressure spikes can cause significant damage. As in our patient, a diurnal curve is also valuable for ruling out IOP spikes during the day.
Patients must also be asked about risk factors for transient hypoxia. Previous episodes of hypotension secondary to major surgery or trauma, chronic anemia, vasculitides, nocturnal hypotension, and sleep apnea have also been implicated as causes of LTG.
The clinical exam can also help provide clues toward a diagnosis. Patients with LTG usually have focal loss of rim tissue, especially inferiorly. There is a greater incidence of optic-nerve hemorrhages and often paracentral scotomas.2
The goal of treatment of LTG is to lower IOP 20% to 30%. The Collaborative Normal-Tension Glaucoma Study showed this goal to be most effective in delaying progression. Topical medical therapy and laser trabeculoplasty can be used as initial treatment. If lower pressures are required, trabeculectomy is the surgery of choice, with anti-metabolite adjuvants when necessary, since setons typically do not provide low enough pressures for patients with LTG.
Finally, given the findings in this case, a comment on sleep apnea as a source of glaucomatous optic-nerve damage is warranted. Several studies in the past decade have looked at the relationship between sleep apnea and POAG and LTG. In several studies, the prevalence of glaucoma in individuals with sleep apnea was reported to be 2% to7%.3,4 The incidence of LTG was noted to be higher.5 The respiratory disturbance index (RDI) is used in sleep studies to grade apnea. An RDI >10 is considered to meet the diagnosis of sleep apnea. The respiratory disturbance index has been shown to correlate positively with IOP, visual field loss variance, glaucomatous optic-disc changes, and the diagnosis of glaucoma. Our patient had an RDI of 44.1. Once he began CPAP treatment, no further glaucoma progression has been noted.
In investigating any patient with LTG, it is important to rule-out possible secondary causes as we have outlined previously. An overlooked cause of LTG may be sleep apnea. Careful patient history can help determine which patients need referral to a sleep study center for polysomnography. Ultimately, patients with LTG may require aggressive medical treatment, and often require trabeculectomy for adequate pressure control.
Case One was submitted by Faris R. Ghosheh, M.D., and Eve J. Higginbotham, M.D., who are affiliated with the University of Maryland's Department of Ophthalmology and Visual Studies in Baltimore, Md.
To comment on this case, e-mail Ophthalmology Management at zummoj@boucher1.com.
References (Case One)
1. Collaborative NTG Study Group. Comparison of glaucomatous progression between untreated patients with NTG and patients with therapeutically reduced IOP. Am J Ophthalmology. 1998;126:487-497.
2. Kent AR. Low-tension glaucoma. In: Higginbothm EJ and Lee DA, eds. Clinical Guide to Glaucoma Management. Woburn, MA: Butterworth and Heinemann; 2004:193-191.
3. Mojon DS and Hess CW. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology. 1999;106:1009-1012.
4. Geyer O and Cohen N. The prevalence of glaucoma in patients with sleep apnea syndrome: same as in the general population. Am J Ophthalmol. 2003;136:1093-1096.
5. Mojon DS and Hess CW. Normal-tension glaucoma is associated with sleep apnea syndrome. Ophthalmologica. 2002;216:180-184.
Case Two: Reversal of cupping following trabeculectomy
Case history presentation: A 75-year-old female was referred for evaluation and treatment of open-angle glaucoma. She had uncontrolled IOP and glaucomatous progression of optic-nerve heads and visual fields on maximal tolerated medical therapy with dorzolamide hydrochloride-timolol maleate (Cosopt), brimonidine tartrate (Alphagan), and latanoprost. She had been treated medically for open-angle glaucoma for approximately 5 years.
Examination:
- Best-corrected visual acuity was 20/30 OD, and 20/25+ OS
- Humphrey visual fields revealed paracentral losses in both eyes, right greater than left
- Anterior segment was remarkable for pseudophakia OD and mild, nuclear sclerotic cataract OS
- Applanation tonometry was measured at 32 mm Hg OD and 31 mm Hg OS
- Fundoscopic examination showed optic-nerve heads with advanced glaucomatous cupping in both eyes. (See images below.)
Treatment: Patient underwent trabeculectomy in the right eye followed by the left eye, attaining stable IOPs in the low teens OU. Postoperatively, persistent reversal of glaucomatous cupping was observed in the left optic disc. (See images.)
Comparison of the pre-op and post-op imaging illustrates the dramatically smaller optic disc cup 18 months following trabeculectomy demonstrating cupping reversal. (See images.)
|
|
|
|
The noted vessel (arrow) illustrates the base of the disc cupping in the preoperative (left) and postoperative (right) optic disc |
|
Discussion:
Optic-nerve-head cupping reversal following IOP reduction has long been recognized in congenital and infantile glaucoma, and to a lesser extent in adult glaucoma. First reported by von Jaeger in 1869, optic-nerve-head cupping reversal in adult glaucoma was reported in recent literature with increasing frequency employing the use of optic-nerve head tomography as objective measures of disc parameters. However, questions remain as to whether this documented reversal represents a stable alteration in the optic-nerve head or simply a transient postoperative change.
|
|
|
|
HRT imaging of the left optic disc at presentation. Images courtesy of Mathew Sapp, M.D. |
|

|
|
|
HRT imaging of the left optic disc at 18 months after trabeculectomy. Images courtesy of Mathew Sapp, M.D. |
Using various imaging modalities, several studies have shown statistically significant reversal of cupping at various postoperative time intervals.1-5 Irak and Raitta noted statistically significant persistence in cupping reversal after trabeculectomy at 3 and 12 months, respectively.1,2 Funk reported cupping reversal in 5 of 18 eyes at 1 year following IOP reduction, and persistence in cupping reversal at 3 years in 2 of the 5 eyes.3 In contrast to these reports, a longitudinal study of optic-disc topography conducted by Topouzis and colleagues noted reversal lasting only 2 weeks after trabeculectomy, becoming insignificant at 4- and 8- month measurements.6 More recently, Kotecha conducted a longitudinal study that observed cupping reversal after trabeculectomy that did not become statistically significant until 2 years postoperatively.5
The different cupping outcomes from the Topouzis study have been attributed to an increase in the degree of glaucomatous optic neuropathy in that study population.6 It was suggested that more advanced glaucomatous damage may be less likely to undergo cupping reversal.3-7 However, this case report suggests that prolonged reversal can be observed in eyes with advanced glaucomatous optic neuropathy.
Cupping reversal has been attributed to edema of the neuroretinal rim, decreased posterior bowing of lamina cribrosa, astrocytic proliferation, and increased intravascular volume. Several studies have suggested an association between degree of reduction in IOP and cup reversal.4,5 Clinical significance of cupping reversal is not well understood; however, there have been reports of visual field improvement paralleling cup reversal.4 Longitudinal studies are still required to determine if reversal of cupping is associated with a beneficial functional outcome. The recent increase in literature on glaucomatous cupping reversal parallels the advances in imaging that aid in the detection and documentation of this phenomenon by providing objective, noninvasive, reproducible, and quantitative measures of the optic-nerve head.
Case two was submitted by Mathew Sapp, M.D., Blythe Monheit, M.D., and Christopher Girkin, M.D., who are affiliated with the University of Alabama at Birmingham, Department of Ophthalmology. Dr. Girkin is a consultant for Heidelberg Engineering and Carl Zeiss-Meditech.
If you would like to comment on this case, e-mail Ophthalmology Management at zummoj@boucher1.com.
References (Case Two)
1. Irak I, Zangwill L, Garden V, et al. Change in optic disk topography after trabeculectomy. Am J Ophthalmol. 1996;122:690-695.
2. Raitta C, Tomita G, Vesti E, et al. Optic disc topography before and after trabeculectomy in advanced glaucoma. Ophthalmic Surg Lasers. 1996;27:349-354.
3. Funk J. Increase of neurretinal rim area after surgical intraocular pressure reduction. Ophthalmic Surg. 1990;21:585-588.
4. Katz LJ, Spaeth GL, Cantor LB, et al. Reversible optic disk cupping and visual field improvement in adults with glaucoma. Am J Ophthalmol. 1989;107:485-492.
5. Shin DH, Bielik M, Hong YJ, et al. Reversal of glaucomatous optic disc cupping in adult patients. Arch Ophthalmol. 1989;107:1599-1603.
6. Topouzis F, Peng F, Kotas-Neumann R, et al. Longitudinal changes in optic disc topography of adult patients after trabeculectomy. Ophthalmology. 1999;106:1147-1150.
7. Kotecha A, Siriwardena D, Fitzke FW, et al. Optic disc changes following trabeculectomy: longitudinal and localization of change. Br J Ophthalmol. 2001;85: 956-961.











