Compression May be Key to Variability in CK Results
NearVision CK LightTouch technique leads to
a more robust effect and less induced cylinder.
BY H.L. "RICK" MILNE, M.D.
Increasingly, data are beginning to support the notion that the amount of corneal compression caused by the surgeon's indentation of the corneal tissue during a conductive keratoplasty (CK) procedure is a major factor in the way the cornea responds.
This explains why some surgeons have gotten the response predicted by the nomogram used in the FDA clinical trials and why others, like myself, got an under-response.
|
|
|
|
In the conductive
keratoplasty pressure technique more tissue will be drawn into the circle of effect from the pulse if there is no other mechanical force acting upon the tissue.(Image courtesy of Rick Milne, M.D.) |
It appears that the more a surgeon indents the cornea at the time of application the less initial response. This began to dawn on me when I heard Glenn Strauss, M.D., describe his standard technique. Dr. Strauss noted that he compresses the cornea with the probe until the ring-light reflex is displaced to the pupil border. In contrast, my technique involved much more vigorous compression, which typically displaced the light reflex beyond the mid-iris.
With this understanding, my technique has evolved in recent months into an application called NearVision CK LightTouch (LT) technique, where I attempt to have minimal to no corneal compression at the time of radiofrequency probe application. The amount of compression applied has become the most important aspect of my technique.
If we look at the theory of CK, it makes sense that variable degrees of compression might yield variable responses. Radiofrequency energy heats tissue. Heated tissue shrinks toward the source of heat. During the 0.6-second CK pulse, more tissue will be drawn into the circle of effect from the pulse if there is no other mechanical force acting upon this tissue. (See image below.)
When we compress the cornea we are causing a mechanical stretching effect on the corneal fibers, which resists the natural tendency of the tissue to be drawn toward the pulse. (See image at the top of page 72.)
This not only explains the varied response to standard CK treatments, it also helps explain the incidence of astigmatism in some surgeons' hands despite an apparently perfect procedure.
Conductive Keratoplasty LightTouch Technique
I use a Strauss marker to mark the spot pattern on the cornea. At each spot, I place the keratoplast tip firmly into the cornea. I apply sufficient pressure to indent the cornea to the point that striae extend to the pupil and the ring-light reflex is displaced away from the probe. I then gradually release the pressure until there is minimal to no indentation of the cornea. Before delivering the radiofrequency energy, I watch for the striae around the probe tip to be less than 1/2 mm and for the ring-light reflex to return to its original position.
|
|
|
|
In the NearVision conductive keratoplasy LightTouch technique, compression of the corneal fibers resists the natural tendency of the tissue being drawn toward the pulse.(Image courtesy of Rick Milne, M.D.) |
|
Surgeons who perform this technique will notice a marked tissue response and a noticeable flattening of the light ring in the sector of the delivered pulse.
In fine-tuning this technique, I've noticed that after the first two spots are placed and the bands between them begin to form, the cornea tends to contract away from the probe with each subsequent spot. When this occurs, I gently follow the contraction to make sure that the probe tip remains properly seated in the cornea. This results in deeper bands and greater stability, and should resolve any problems with regression experienced upon first attempting this technique.
I would also caution that it is important to coach the patient not to move during the treatment. This technique gives the surgeon less control over the probe should the patient move during application.
With the LT pressure technique, the standard CK nomogram will yield dramatic over-treatment, so a more conservative approach is required. The first time I attempted to perform CK with very little pressure, I used the standard nomogram, applying 16 spots at 6 mm and 7 mm, for a 48-year-old plano presbyope. One week post-op, the patient was -4.25D. Surgeons new to this technique must plan to use fewer spots and treat at a larger optical zone.
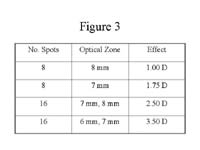
My current nomogram (See table above.) is what I use for all virgin corneas, previous CK-treated eyes, and hyperopic LASIK/PRK patients, without adjustments. The variability of response is 0.50D. I use a +1.00, +1.75, and +2.50 loose lens to determine the amount of correction needed.
I am very cautious in treating previous myopic LASIK/PRK patients. In these patients, I still use the CK LT technique, but I begin at 9 mm, with a warning to the patient that they might need an enhancing ring later.
|
|
|
|
The Milne Nomogram, which is currently being used by Dr. Milne for all virgin corneas, previous CK-treated eyes, and hyperopic LASIK/PRK patients, without adjustments. Nomogram courtesy of Rick Milne, M.D. |
Results
I have treated approximately 200 eyes over 9 months using the CK LT technique and nomogram described previously. Thus far the initial response is very robust, with no apparent loss of stability compared with conventional CK. I have needed to enhance less than 5% of cases for under- responding or induced astigmatism.
The incidence and degree of induced astigmatism is greatly reduced with the CK LT technique. This technique reduces the need for balancing spots and improves patient satisfaction with the procedure.
One of the most exciting aspects of this technique is that it provides the same post-op "wow factor" that LASIK patients experience. A 48-year-old female, who I recently treated, is a good example. Preoperatively, her reading vision was J16 OU with 20/60 spectacle-corrected distance visual acuity. Just 10 minutes post-op, she was 20/15 and J3 in the distance eye and 20/40 and J1 in the near eye.
When there is some induced cylinder, I have elected to treat it at 1 week post-op with the balancing spot being placed on the axis of the minus cylinder. I place one spot for every diopter of correction needed, although I do not enhance if there is less than 1.50 D of induced cylinder because it usually regresses over time.
I would caution that the CK LT technique is an off-label use of CK and that long-term regression of the CK LT technique is unknown, although my unpublished data suggest it is no greater a regression than with conventional pressure CK.
Also, if you treat with more than a 1.00D response (8 spots at 8 mm) you should preoperatively counsel the patient about monovision. However, in my experience the monovision symptoms that one sees above +1.00D usually resolve over the first 3 months, evolving to a more blended vision effect. Patients maintain their near vision ability, while the distance vision and monovision symptoms improve.
Re-treatments
I have re-treated patients who had an initial under-response to traditional CK with the CK LT technique and had a very robust initial response in these nonvirgin eyes. As noted previously, I do not change my CK LT nomogram at all for these prior under-responders, and have achieved well past the former +0.75D barrier for re-treatment.
I do most re-treatments under the operating microscope with LightTouch CK. The slit lamp can be used in such cases, but it can be more difficult with LT because the patient is more likely to move his or her eyes when seated upright at a slit lamp.
I mark two consecutive spots under the slit lamp, and then place an additional two spots along an imaginary line extending from the center of the pupil onto the sclera. I use these as reference points for alignment of the Strauss marker.
Occasionally, I have treated a patient with the CK LT technique who still under-responded. If the refraction is stable, I re-treat at 6 months using the loose lens test and my same nomogram. I do expect, however, to see about 0.25D to 0.50D less response than in a virgin eye. Photorefractive keratoplasty is also an option.
An over-response may be more common with the CK LT technique. I would recommend that no re-treatment of these patients be done for at least 6 months, and if they are having documented CK regression at 6 months I would wait at least 1 year.
I treat these patients who have over-responded with PRK without Mitomycin C and have experienced good results with no haze. I would not recommend LASIK because the flap going through the CK treatment columns can give a less predictable result.
I fully expect that our nomograms, expectations of the procedure, and recommendations for enhancing over- and under-responses will change as we gain more experience with this technique. NearVision CK LT is an evolving procedure, but the prospects for better and more predictable results with the CK LT technique are exciting to me.
H.L. "Rick" Milne, M.D., is the president of The Eye Center, PA in Columbia, S.C. Dr. Milne can be reached at (803) 256-0641 or hmilne@aol.com.
Dr. Milne is a consultant to Refractec, Inc. He has no financial interest in any of the information contained in this article.