Surgical Pearls for
Refractive Lens Exchange
Minimally invasive techniques
lead to the best outcomes.
BY I. HOWARD FINE, M.D.
|
|
|
|
A bimanual microincision technique with separate irrigation and aspiration works well in removing the relatively soft lenses usually encountered in refractive lens exchange patients. Here, the nucleus is being carouseled with the irrigator and the phaco tip in the plane of the
capsulorrhexis. Source: I. Howard Fine, M.D. |
|
Refractive lens exchange (RLE) has proven to be a safe, reliable option for the correction of presbyopic hyperopia and carefully selected patients with myopia, especially with the implantation of a multifocal or accommodating IOL. Experience has shown us some special approaches for achieving the best results after RLE:
Make the incisions with care. I prefer to use a bimanual microincision technique with separate irrigation and aspiration for lens removal, even in my routine cataract cases. This technique works especially well on the relatively soft lenses usually encountered in RLE.1, 2
The surgeons in our practice always use trapezoidal diamond blades to make the clear corneal incisions in these cases. The incisions are made 1.5 mm long, have an internal width of 1.0 mm, and have an external width of 1.2 mm.
The instruments are placed so as to straddle the temporal periphery, with the irrigator in the left hand and the phaco needle in the right. The left-hand paracentesis is made almost horizontal at about the 7:30 clock position, and the right-hand incision is almost vertical at about 5 o'clock. Because the two incisions are almost at right angles to each other, we can use the irrigator as a lens manipulator with no distortion of the wound as the irrigator and phaco needle are brought together.
Keep the irrigator in place throughout the procedure. Once we have the irrigator in the eye, we never take it out. This keeps the anterior chamber formed throughout the procedure. The corneal incisions are small and self-sealing, so there is no anterior chamber evacuation as they are created or while we irrigate paraben-free lidocaine into the anterior chamber. An injection of viscoelastic then keeps the chamber stable as the capsulorrhexis is created and as the various "hydro" steps are performed (as described below).
|
|
|
|
|
|
|
Results of refractive lens exchange with implantation of the Array multifocal IOL. Top: Attempted vs. achieved spherical equivalent refraction in 144 eyes demonstrated very good predictability. Bottom: Postoperative uncorrected visual acuity with near vision measured monocularly and distance vision measured binocularly. Source: I. Howard Fine, M.D. |
|
The irrigator remains in place while the phaco tip is being used, during the time when the phaco tip is exchanged for an aspiration tip to polish the capsule and remove any residual cortex, and even when the aspiration tip is removed and additional viscoelastic is injected into the capsule. Only then do we remove the irrigator, create a new incision between the first two, and implant the intraocular lens.
Keeping the irrigator in place this way ensures that the vitreous face is never permitted to come forward during surgery. This prevents shallowing of the anterior chamber and the transfer of stress to the vitreous base.
Approach soft lenses differently. The relatively young patients who are often candidates for RLE tend to have soft lenses. Soft lenses are easily deformable, so they behave quite differently from cataractous lenses, but they can be readily removed with bimanual microincision surgery.
We perform cortical cleaving hydrodissection routinely. Depending on the size of the capsulorrhexis, this is followed by hydrodelineation if the lens is somewhat firm. We do not use hydrodelineation in very soft lenses.
The lens is then hydroexpressed out of the capsule so that we can carousel it in the plane of the capsulorrhexis. (See image on previous page.) With the irrigator in the left hand coming in horizontally and the phaco needle in the right hand with the bevel facing the equator of the hydroexpressed lens, we carousel it, rotating and aspirating to remove lens material from the outside in. This can be accomplished without any ultrasound in almost all cases. The use of cortical cleaving hydrodissection leaves us with very little cortex at the end of the case.
The technique is slightly different when we are using the crystalens accommodating IOL, which requires a 4-mm capsulorrhexis. There is always residual epinucleus in the capsule in these cases because only the endonucleus can be hydroexpressed through the smaller opening, even with a soft lens. The epinucleus is trimmed and flipped in the usual manner.
The Overall Approach
These methods form part of the overall approach that leads to successful RLE, which is to perform minimally invasive surgery. By removing the lens with fluidics only and no ultrasound energy, and by working in the safe zone midway between the posterior capsule and the cornea, the procedure has minimal risk.
This approach has provided excellent outcomes for our RLE patients receiving the Array multifocal IOL or the crystalens, as shown in the accompanying slides.
|

|
|
|
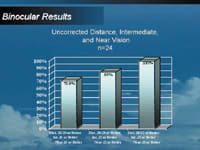
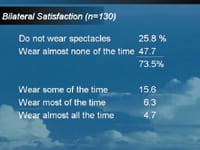
Results of refractive lens exchange with implantation of the crystalens accommodating IOL. Top: Binocular uncorrected visual acuity in refractive lens exchange patients implanted with the crystalens. Center: Percentage of patients in the FDA-monitored study with bilateral crystalens implants and levels of uncorrected postoperative distance, intermediate, and near visual acuity. Bottom: Patient-reported spectacle use after crystalens implantation. Source: I. Howard Fine, M.D. |
||
I. Howard Fine, M.D. is a clinical professor of Ophthalmology at the Casey Eye Institute at Oregon Health & Science University in Portland and in clinical practice with Drs. Fine, Hoffman & Packer, LLC, in Eugene, Ore.
References
1. Fine IH, Hoffman RS, Packer M. Optimizing refractive lens exchange with bimanual microincision phacoemulsification. J Cataract Refract Surg. March 2004;30(3):550-4.
2. Fine IH, Hoffman, RS, Packer M. Clear lens extraction with multifocal lens implantation. International Ophthalmology Clinics: Presbyopia. MH Friedlaender (ed.). Lippincott Williams & Wilkins, Philadelphia, PA. Spring 2001; 41(2):113-122.











