Making the Most of
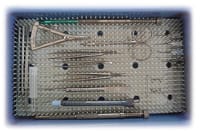
Your Cataract Surgical Tray
BY CHRISTOPHER KENT, SENIOR ASSOCIATE EDITOR
(Following each instrument, we've listed the source from which the practice originally obtained the instrument. All listed instruments are currently available, and many can be obtained from a variety of suppliers in addition to the company listed.)
Bradley C. Black, M.D. (Jeffersonville, Ind.)
Main tray:
- phaco handpiece with sleeve (Bausch & Lomb)
- I/A handpiece with sleeve (Alcon)
- chopper (ASICO AE 4284)
- Unfolder Silver-T lens injector (AMO)
- Unfolder Emerald lens injector (AMO)
- curved tying forcep (Millennium Surgical)
- Utrata forcep (Bausch & Lomb)
- 0.12-mm forcep (Millennium Surgical)
- Castroviejo caliper straight (Millennium Surgical)
- drape scissors (Millennium Surgical)
- Sinskey hook (Bausch & Lomb)
- hydrodissection cannula 25g (Bausch & Lomb)
- speculum (Bausch & Lomb)
- hydroexpression cannula (BD Visitec)
Reason for selection of instruments: The contents of our main instrument tray are largely determined by my surgical preferences; I favor one-handed techniques and use of a peribulbar block. Also, we always work to simplify the tray; we remove any instruments not used in every case.
Arrangement of tools: We arrange the instruments in the exact order we use them and immediately place them back after usage. This makes it easier for the scrub to just "go down the line."
For more complex surgery: Unusual cases are identified pre-op and any special instruments are noted when scheduled and ready on the table (e.g., chopper, pupil dilator, capsular tension ring, Healon5).
For unexpected complications: We keep separate instruments such as tiers, needle holders and vitrectomy sets sitting nearby in the room in peel-packs for rapid utilization.
Managing flow: We do six cases an hour out of two ORs using four sets of instruments and two or three sterilizers; the trays are ready in 6 to 8 minutes. We can do seven or eight cases per hour when no complicated cases are mixed in.
Michael P. Graham, M.D. (Orlando, Fla.)
Main tray:
- curved iris scissors (Bausch & Lomb)
- Lancaster lid speculum (Bausch & Lomb)
- Utrata forcep (Bausch & Lomb)
- Colibri 0.12-mm forceps (Bausch & Lomb)
- 2 McPherson tying forceps (Bausch & Lomb)
- 0.5-mm toothed forceps (Bausch & Lomb)
- small Westcott scissors (Bausch & Lomb)
- Vannas scissors (Bausch & Lomb)
- McPherson small needle driver (Weck)
- 3-mm diamond keratome (multiple sources)
- 15° blade on a Beaver holder (multiple sources)
- Grayson nucleus manipulator, for chopping softer cataracts (Bausch & Lomb)
- Lester hook (Katena)
- spatula, used as a second instrument for divide and conquer phaco (Moria)
- Conner wand (Rhein)
- various cannulas
- I/A handpiece with interchangeable angles and 180° tips
- bent 25-gauge cystotome needles (we bend our own)
Reason for selection of instruments: Our tools are selected to accommodate several surgeons. (For example, I don't use the Utrata forceps to open the capsule, but one of my partners does.) We're planning to add a Nichamin chopper, which I prefer to use with harder cataracts.
Arrangement of tools: The instruments are arranged in the order we use them. The iris scissors (to cut the drape) and speculum are in the front; instruments rarely used are in the back. Any instruments used exclusively by surgeons not operating that day are moved to the back of the tray.
For more complex surgery: We have extra instruments on another tray for times when more complicated surgery is planned. This tray is kept in a small prep room next to the OR, easily accessible.
Managing flow: Each of our surgeons works in two ORs with four instrument trays. One tray is in the room currently in use, another is being opened in the next room, and two are being autoclaved. One of those two will be brought in when the surgeon leaves the current room. The other provides spare instruments in case of damage or contamination. With this setup we can do five cases an hour -- six if we're really on a roll.
Bradford
Shingleton, M.D., (Boston, Mass.)
Main tray:
- blunt Westcott drape scissors (Bausch & Lomb)
- Steinert-Lieberman nasal lid speculum (Rhein)
- Sharpoint 2.85 clear cornea steel keratome (Surgical Specialties)
- Sharpoint paracentesis 15° stab blade (Surgical Specialties)
- bent 25-gauge capsulorhexis needle (we bend our own)
- Wiles hydrodissection cannula (Bausch & Lomb)
- titanium capsulorhexis forceps (Rhein)
- Simcoe I/A cannula (Bausch & Lomb)
- Hoskins forcep (Katena)
- Bishop-Harmon 19-gauge irrigation cannula (Oasis)
Reason for selection of instruments: We systematize our procedures so that we can use the smallest number of instruments possible. We change the lineup whenever there's a technique or equipment modification in our OR.
Arrangement of tools: Because we use so few tools, the layout on the tray isn't really an issue. Usually the scrub simply makes sure that everything is easily visible, rather than trying to lay the instruments out in order of use.
For unexpected complications: We keep a needle-holder, McPherson tying forceps, long-angled Vannas scissors, astigmatic keratotomy blades and iris retractors in the room, wrapped individually, in case they're needed. (We do our best to identify cases in which stitches may be needed ahead of time, so the appropriate instruments can be added to the tray before the case is started.) We have a sterilized extra-cap setup available, kept in a separate room, for the rare instances when conversion is necessary.
Managing flow: We work out of two ORs using four trays -- two for each room. One is in use while the other is being sterilized. I can perform about six uncomplicated phacos per hour with this arrangement, without rushing or putting pressure on the staff.








