Taking
IntraLase To the Next Level
The femtosecond laser's newer 15-kHz engine allows for quicker flap creation, with more predictable dimensions and easier-to-lift flaps.

Refractive surgeons recognize the importance of flap architecture in achieving optimal LASIK outcomes. A growing number of surgeons find they can create smooth, predictable flaps with virtually no corneal complications using the IntraLase femtosecond (FS) laser.
Now, with the newer 15-kHz unit, I can create flaps more quickly, with a narrower thickness range and reduced standard deviations than those of the older 10-kHz model. Recent studies in my office and elsewhere have confirmed these and other findings, demonstrating the advantages of using the IntraLase laser to create LASIK flaps. In this article, I'll describe these studies and their implications for clinical practice.
Comparing the two engines
I initiated a prospective study to determine flap dimensions and clinical outcomes with the IntraLase FS laser, using both the 10-kHz engine released in 2002 and the speedier 15-kHz engine launched last year.
With the 15-kHz engine, I can create a 9-mm flap in 50 to 57 seconds compared with 90 to 110 seconds with the older engine. One can increase the speed of the flap creation by putting the laser spots farther apart or by decreasing the diameter of the flap. On the other hand, changing the angle of your side cuts from 90º to 30º prolongs the time for flap creation. Basically, you trade speed for smoothness. For most of my cases, I use 10-µm x 10-µm spot settings and side cuts of 30º to 55º.
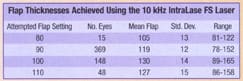
Looking at my results with the 10-kHz IntraLase engine, it's worth noting that the attempted flap thickness is not what I measure (see "Flap Thicknesses Using the 10-kHz IntraLase Laser"). While I attempted to create a 90-µm flap by dialing in the 90-micron setting, in most of my cases, my mean achieved flap thickness was 119-µm. My standard deviations were roughly half of what I achieved with mechanical microkeratomes. The ranges of flap thickness were narrower as well.
Next, I compared these results with those I obtained using the 15-kHz IntraLase engine (see "Flap Thicknesses Using the15-kHz IntraLaseLaser"). In both the 90-µm and the 100-µm attempted flap settings, the mean standard deviations and ranges using the 15-kHz engine were better than those of the 10-kHz engine.

The 15-kHz IntraLase engine offers other advantages over the 10-kHz model. The newer engine:
- Makes it easier to lift the flap (a pleasant surprise).
- Induces less trauma.
- Lets me move faster than before (which may in part account for the improved results).
Clinical outcomes
Overall, complications using the IntraLase FS laser were minimal. I had several slipped flaps by the end of the study when I discovered that phenylephrine was causing a loss of endothelial cell pump function. I had one case of visually insignificant striae. Facilitating matters is the fact that flaps made with the IntraLase laser are parallel faces with a relatively uniform thickness, which has the advantages of flap stability and possibly fewer and more predictable wavefront aberrations.
In my experience to date, I've had no epithelial defects in more than 1,000 eyes treated using the IntraLase FS laser. Separate studies by Jonathan Christenbury, M.D., Karl Stonecipher, M.D., and Brian Will, M.D., likewise found no epithelial defects in eyes treated with the IntraLase unit. This comes as no surprise, since you're not moving anything over the eye. This also means that map-dot-fingerprint dystrophy is not a contraindication to LASIK using the IntraLase laser.
Wishing to determine whether the thinner Intralase flaps affected best spectacle-corrected visual acuity (BSCVA), I performed a retrospective comparison of eyes treated with the Bausch & Lomb ACS microkeratome, the Alcon SKBM microkeratome and the IntraLase FS laser. For this study, I looked at flaps less than 500 microns thick. Among eyes with a preoperative refractive error of 1.00D to 3.00D, 1.7% of those treated with the IntraLase laser lost two lines of BSCVA and no eyes lost more than two lines. None of the IntraLase eyes with a preoperative refractive error of 3.00D to 9.00D lost two or more lines of vision. These data compare favorably with those of the ACS and the SKBM, which produced minor, but greater incidences of two or more lines of BSCVA lost.

Clinical advantages
Among the virtues of the 15-kHz IntraLase engine is its speed, which has reduced my flap time from as high as 110 seconds to 57 seconds for a 9-mm diameter flap. A pleasant surprise is how easily I can lift the 15-kHz flap compared with the flap created with the 10-kHz engine.
The predictability of the flap dimensions is superior to that of mechanical microkeratomes; you can reduce the standard deviation of your flap thicknesses by half, compared with those of a mechanical microkeratome, and narrow your range by 40% to 50%. This means you can operate on higher myopes whom you might not have treated before. You can leave thicker postoperative stromas; I'm leaving 300 µm to 325 µm on a routine basis. Most importantly, flap creation is safer than with mechanical microkeratomes because the IntraLase is not sensitive to preoperative corneal curvature and corneal thickness.
Dr. Binder is the co-medical director for IntraLase Corp. He practices in San Diego, at the Gordon Binder Vision Institute. He is past President of the International Society for Refractive Surgery, CLAO and The International Society for Contact Lens Research.
|
ASSESSING THE ALTERNATIVE: MECHANICAL FLAP CREATION |
While evaluating the relative merits of the IntraLase femtosecond laser, consider the current standard method of flap creation using a mechanical microkeratome. The factors that determine its outcomes and the catalogue of complications have been well-described. Many variables affect how you create a LASIK flap using a mechanical microkeratome. Among these are the oscillation of the blade, the means by which you fixate the microkeratome to the eye, your vacuum settings and whether or not you applanate the cornea as translation occurs. Also figuring into the equation are the means of advance (direct-driven, spring-driven, manual), whether or not you have a view of the process, whether you can control your diameters and thicknesses, whether you have back-up power and whether you have audible feedback to indicate the location of the blade. Beyond that, numerous factors affect the flap's dimensions. One is the quality of your blade; with each successive use, you get thinner flaps. The blade's oscillation -- from 6,000 cpm up to 20,000 cpm -- affects the smoothness and quality of the cuts. Another factor is the translation speed; a faster advance creates a thinner cut. Other factors come into play. Variations in the gap's width can produce flaps of varying thickness, giving you wide ranges and standard deviations. The play of the blade moving within the gap across the eye likewise affects the flap's thickness. The corneal thickness and the power are additional variables; thicker corneas give you thicker flaps, while steeper corneas yield thinner flaps. These factors affect the flap's diameter as well. There's also the matter of the machine's suction. Does the suction ring have one, two or multiple ports? You want to avoid altering the IOP as you're translating across the eye. Mechanical microkeratomes can give rise to a range of problems. Epithelial defects occur in a fixed percentage of cases. A study published in 2001 by Ronald Krueger, M.D., found that the Bausch & Lomb Hansatome produced epithelial defects in 26 of 403 eyes (6.54%), while seven (2.23%) epithelial defects of 314 eyes occurred with the Moria CB unit, one of 147 (0.68%) with the Moria M2 and one of 134 (0.75%) with the Alcon Lasitome. A study by Karl Stonecipher, M.D., and Guy Kezirian, M.D., noted loose epithelium in 7.7% of Hansatome-treated eyes, 9.6% of Moria CB eyes and none of the IntraLase eyes. We've all had problems with interface inflammation (diffuse lamellar keratitis) as well as slipped flaps. With the laser you can't lacerate a cap during the pass if you lose suction, as happens with mechanical microkeratomes; the laser focuses immediately to the surface. With mechanical microkeratomes, you can get free flaps, partial flaps and irregular flaps. In some cases, you might risk penetrating the anterior chamber. Other times, you may decenter the flap. If the microkeratome's cam breaks, the blade can lose power and stop. Cap perforations (buttonholes) rarely occur; I've had seven or eight in more than 8,000 eyes treated with a mechanical microkeratome. None of these complications have occurred in my series with the IntraLase.
|
This is one of a series of articles recapping presentations given at the IntraLase booth during the 2003 meeting of the American Academy of Ophthalmology.
SPONSORED BY









