Glimpsing the Future
of LASIK With ESP
Testing the Efficiency, Safety and
Predictability of IntraLase vs.
conventional microkeratomes.

Do laser incisions make a difference in LASIK outcomes? To study the efficiency, safety and predictability of mechanical microkeratomes versus the IntraLase femtosecond (FS) laser, my colleague, Guy M. Kezirian, M.D., and I compared conventional LASIK outcomes achieved using the IntraLase laser with those achieved using two mechanical keratomes. During our study, we treated a total of 375 eyes: 126 with the Moria CB keratome, 143 with the Hansatome and 106 with the IntraLase FS laser.
|
|
|
The IntraLase FS laser consistently created predictably thinner flaps. |
Study cohorts were similar for all flap modalities, which were categorized according to mean preoperative spherical equivalent and mean preoperative pachymetry. After surgery, we evaluated flap thickness, degree of loose epithelium, incidence of device failures, change in best-corrected visual acuity (BCVA) and occurrence of buttonhole or torn flaps. This article presents some of our findings.
Predictable flap thickness
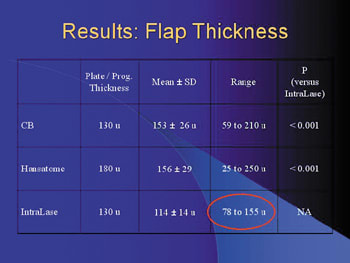
Most of us will agree that the riskiest aspect of LASIK is creating the corneal flap. Ideally, we want to use a device that produces flaps of predictable size and thickness. To evaluate the reliability of two mechanical keratomes and the IntraLase FS laser, we compared target and observed flap thickness in our study population. Target thickness was 130 µm for the CB, 180 µm for the Hansatome and 130 µm for the IntraLase FS laser. With a mean standard deviation of 14 µm, the IntraLase FS laser created a tighter range of predictably thinner flaps than the CB and the Hansatome, which had mean standard deviations of 26 µm and 29 µm, respectively. (For more details, see "Results: Flap Thickness.")

Preserving epithelial integrity is important for successful post-LASIK healing. In our study, we used Daniel S. Durrie, M.D.'s four-grade system to categorize the degree of loose epithelium in our patients.
None of our patients fit criteria for Grade III (loose epithelium in three quadrants) or Grade IV (complete slough). However, as illustrated by the chart on this page, 9.6% of CB patients, 7.7% of Hansatome patients and 0% of IntraLase patients showed Grade I (one quadrant) or Grade II (two quadrants) loose epithelium. These results suggest that patients treated with the IntraLase FS laser may heal faster, reducing their risk of developing diffuse lamellar keratitis, epithelial ingrowth and flap striae. I've even used the IntraLase FS laser to treat 26 map-dot fingerprint dystrophy patients (not included in this study cohort) without compromising their epithelial integrity.

If we look at 1-day post-op vision, all three devices had similar rates of 20/20 acuity. IntraLase patients had a slightly lower, but not statistically significant, 20/20 rate. At 3 months, there were no statistically significant differences among the groups.
Since this study, I've modified my preoperative routine for IntraLase patients. Placing patients on a regimen of preoperative ophthalmic steroids and antibiotics has significantly reduced the incidence of 1-day post-op inflammation and edema. As a result, my 1-day post-op 20/20 rates have increased to about 78%.
Sphere and cylinder outcomes
The manifest spherical equivalent in the +/-0.5 range was better with the IntraLase FS laser than with the CB and the Hansatome keratomes (see "Manifest Spheroequivalent"). The same data plotted on a spherical equivalent scattergram, shows that the IntraLase FS laser is comparable to the Hansatome (see "Spheroequivalent Scattergrams").

Seeing the future
Our research shows that the IntraLase FS laser offers more predictable flap thickness, better epithelial preservation, refractive predictability and neutral cylinder outcomes. During our study, we noted no significant difference in the distribution of changes or mean change in best spectacle-corrected vision. We experienced no device failures and noted no buttonholes or torn flaps among patients treated with the three devices.
We're currently studying how the IntraLase FS laser affects the outcomes of wavefront-guided ablations. We all want a more predictable flap, better epithelial preservation and better refracted scattergrams. I think we'll achieve these goals with the IntraLase FS laser.
Karl G. Stonecipher, M.D., practices at Southeastern Eye Center in Greensboro, N.C.
SPONSORED BY

This is one of a series of articles recapping presentations given at the IntraLase booth during the 2003 meeting of the American Academy of Ophthalmology.








