Troubleshooting PHACO
Tips for making cataract surgery go smoothly.
With intraocular lens technology rapidly evolving and Baby Boomers aging, cataract surgery may soon be in its heyday. With that in mind, we asked a number of experienced surgeons to share ways they've learned to resolve -- and prevent -- problems during phaco.
|
|
|
|
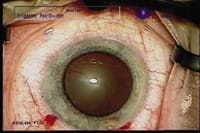
Pupil dilation is maximized 60 seconds after injection of 1% lidocaine
MPF |
|
Avoiding pupil constriction. Despite adequate dilating drops and epinephrine in the infusion fluid, a pupil may gradually constrict during cataract surgery, making completion of the procedure difficult or impossible. However, before resorting to iris retractors, try injecting 0.2 to 0.4 cc of lidocaine MPF 1% (already used in many patients as an adjunct to topical anesthesia). This paralyzes the iris sphincter muscle that causes the pupil to constrict, allowing the pupil to re-dilate.
I've found that this method works quite well; in fact, I no longer use dilating drops in any of my routine patients. Instead, I inject the lidocaine at the beginning of the procedure, which allows the pupil to dilate within 60 to 90 seconds. Instilling viscoelastic mechanically enlarges the pupil further. This strategy has several advantages:
- The corneal epithelium isn't challenged by the instillation of drops or an ointment containing preservatives.
- Because pupil diameter is small at the start of surgery, the patient is much more tolerant of the microscope light as the procedure begins.
- The patient doesn't have to come to the operating facility an hour or more before surgery because there's no need to wait for the pupil to dilate.
- The pupil usually returns to normal size and reactivity within 2 hours after surgery, giving the patient better vision more quickly and eliminating complaints of halos around lights the evening after surgery.
- few other important notes:
- Buffer the lidocaine with sodium bicarbonate to make injection more comfortable for the patient. Mix 15 ml BSS and 3.75 ml NaBicarb 8.4%. Withdraw 15 ml of the solution and add 5 ml Xylocaine 4%. (Suggestion originally made by Dr. Lisa Arbisser.)
- If a pupil doesn't dilate well with routine dilating drops, intracameral lidocaine won't be able to provide greater dilation.
- In some patients, intracameral lidocaine may not dilate the pupil as widely as routine dilating drops. (We're currently comparing maximal pupil dilation using these two methods, in collaboration with Dr. Alan Crandall at the Moran Eye Center in Salt Lake City.)
-- Robert J. Cionni M.D., Cincinnati, Ohio
Managing iris prolapse. On rare occasions you may encounter such severe positive pressure that it's virtually impossible to introduce the phaco tip without causing the iris to prolapse into the incision. To facilitate atraumatic entry when iris prolapse is present:
- Aspirate the viscoelastic material from the anterior chamber through the second incision to reduce IOP in the anterior segment.
- Inject Healon5 onto the subincisional iris, gently repositioning it to create vital space.
- Introduce the phaco tip dry -- without any infusion, which would cause the iris prolapse to recur.
Once the ultrasound tip has advanced into the central anterior chamber, initiate infusion and you can safely begin emulsification.
-- Robert H. Osher, M.D., Cincinnati, Ohio
|
|
|
|
Viscodissection can be used to separate tissue when I/A is risky. |
|
Using visco to separate tissue. Viscodissection can save the day as an alternative to I/A when you need to separate tissue. I've used this technique to separate iris from capsule (as in synechiolysis); to separate epi-nucleus from the bag for posterior polar cat-aract (see photo, above); and to separate cortex from the bag before implanting the IOL. This is especially helpful when positive pressure pushes the posterior capsule forward and makes I/A risky.
-- Mark Packer, M.D., Eugene, Ore.
|
|
|
|
Mackool titanium capsule retractors support the bag in the area of a traumatic zonular dialysis. |
Managing CTR placement. With the recent FDA approval of the Morcher Capsular Tension Ring (CTR), U.S. surgeons have a new option to help preserve the capsular bag during phacoemulsification in the presence of weakened zonules. Surgical maneuvers such as sculpting and nuclear rotation exert stress against focal areas of zonules; CTRs redistribute these forces across all 360° of the zonular apparatus.
You can insert the CTR at any time after completion of the capsulorhexis. However, the broad circumferential contact of CTRs within the capsular fornices tends to impede the removal of the epinucleus and cortex. As an alternative to early CTR placement, you can use self-retaining capsule retractors, such as those designed by Richard Mackool (Capsule Support System, Duckworth & Kent) or Ike Ahmed (Capsular Tension Segments, Morcher), to stabilize the capsular bag during nuclear and cortical removal. These retractors don't entrap the cortex to the extent that a CTR does. This strategy will allow you to delay CTR insertion until after cortical I/A has been completed.
-- David F. Chang, M.D., Los Altos, Calif.
(Dr. Chang has no financial interest in any product mentioned.)
|
|
|
|
Timing and the right tool improve limbal relaxing incision outcomes. |
|
Maximizing limbal incision healing. Many surgeons use limbal relaxing incisions to manage co-existing astigmatism at the time of cataract surgery. However, most perform the procedure using a simple groove blade, and many do so after the surgery. We use the ap-propriate Terry-Schanzlin Astigmatome blade (the one that corresponds to the pachymetric reading) to make the limbal incisions before making the paracentesis incision. Because the eye is at its normal pressure before the surgery, the incisions are not only deep, arcuate and precise, they have integrity that ensures normal healing.
-- Edward D. Glinski, D.O., M.B.A.,
Oklahoma City, Okla.
(Dr. Glinski has no financial interest in the Astigmatome or its manufacturer.)
|
|
|
|
Increased endocapsular pressure can cause radial extensions
in the anterior lens capsule. |
|
Managing high endocapsular pressure. The milky, intumescent variety of white cataracts more commonly found in younger patients can be especially challenging because they're accompanied by increased endocapsular pressure. In this situation, the initial puncture into the central anterior lens capsule with the needle cystotome lets fluid enter the lens, causing lenticular swelling and elevating endocapsular pressure. This generates forces on the capsule that can produce radial extensions out to the lens equator in two directions, forming an ominous "minus." (See image, facing page, bottom right.)
To manage this problem, use the needle cystotome to make two additional cuts in the anterior capsule centrally and perpendicular to the tear on both sides, forming a "plus." This helps to disperse the forces and ensure that the opening is large enough for the lens to be removed without a completed capsulorhexis.
With the bottle height lowered and decreased flow rates, introduce the phaco tip and gently aspirate the fluffy white material to reduce the endocapsular pressure. Then impale the lens centrally with high vacuum and prolapse the distal pole out of the bag. Perform phaco chop at a supracapsular level to remove the lens material.
This approach preserves the integrity of the posterior capsule, truly turning a minus into a plus!
-- Rex C. Hsei, M.D., Santa Cruz, Calif.
(Dr. Hsei has no financial interest in any of the technology mentioned.)
Preventing anterior chamber over-deepening. The cause of over-deepening of the anterior chamber (most noticeable in detachment-prone myopes) has been postulated to be the result of the pupil edge making 360° contact with the anterior capsule flap, preventing fluid from distributing between the anterior and posterior chambers. To prevent this in an at-risk eye (i.e., pars plana vitrectomy, loose zonules or myope):
- place a bolus of viscoelastic between the iris and the capsule at 1 or 2 clock hours just after hydrodissection and before entry with the phaco tip.
- Lower the bottle upon initial entry so the rush of fluid into the anterior chamber is less forceful.
- As soon as equilibrium is established, raise the bottle to its normal level.
If the ophthalmic viscosurgical device (OVD) isn't effective in preventing reverse block, try insinuating the tip of the non-dominant hand instrument between the pupil edge and the anterior capsule. As you lift the iris away from the surface of the capsule, the chamber will shallow to a more appropriate depth. (In rare cases this can be segmental, and you may need to lift in more than one quadrant.)
This maneuver should lead to more comfortable patients intra-operatively, quieter eyes peri-operatively and, possibly, fewer long term retinal sequelae.
-- Lisa Brothers Arbisser, M.D., Davenport, Iowa
|
|
|
|
In a very hard nucleus a small trough may help the chopping process. (Note the large stained
capsulorhexis.) |
Managing a mature cataract. To perform emulsification of a nuclear mature (brown or black) cataract:
- Use a dispersive viscoelastic.
- Use capsular dye for the capsulorhexis.
- Make the capsulorhexis slightly larger than usual (about 5.5 mm).
- Perform gentle hydrodissection -- in many cases, the capsule will have thinned.
- Perform phaco chop, chopping the nucleus into multiple small segments before attempting to remove them. This destroys nuclear rigidity and creates enough room to separate leathery nuclear segments.
- Elevate nuclear fragments to the iris plane for emulsification, especially for removal of the final segments. In these cases there's often little cortex to hold the shape of the capsular bag and prevent trampolining of the posterior capsule.
-- William J. Fishkind, M.D., F.A.C.S.,
Salt Lake City, Utah
Using power level effectively. Always vary power according to the density of the cataract. For example, a soft cataract can be removed with 10% of full power, while a hard cataract may require 70%. Some surgeons use one setting for everyone, using a "light foot" for softer cataracts. However, with most instruments this technique results in a loss of vacuum. Also, using power that's too high can cause dangerous surges and requires quicker reactions. This makes surgery less of a pleasure and more of a challenge.
The vacuum created by lower power is also very important when it comes to removing the quadrants. Lower power settings usually allow the cataract to engage with less cutting, so the vacuum is more effective in sucking the cataract from the periphery. For example, if I normally use a setting of 30 or 40 for an average-density cataract, I might lower it to 20 to remove the quadrants, keeping the vacuum fairly high and flow slightly lower (perhaps between 25 and 30). This allows me to purchase well without risking a surge.
-- James Gills, M.D., Tarpon Springs, Fla.