The IntraLase Advantage
A study found that visual outcomes of
IntraLase-treated eyes at 1-day post-op surpassed those of eyes treated with the Hansatome
microkeratome.
When my associate and I started using the IntraLase femtosecond laser to create LASIK flaps in May 2002, we weren't quite sure what to expect. We'd heard from other IntraLase users that in cases where the bed was a little rough, vision sometimes was slightly compromised at 1 day and only improved after 1 to 3 weeks.
In our experience at the Saddleback Eye Center in Laguna Hills, Calif., we soon achieved smooth beds and found that most patients were seeing great at 1-day post-op.
We decided to compare the visual outcomes of LASIK using the IntraLase FS laser vs. the Bausch & Lomb Hansatome microkeratome.
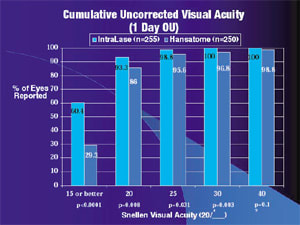
Visual outcomes
At 1 day, 60% of patients treated with the IntraLase unit achieved 20/15 or better uncorrected visual acuity with both eyes vs. 29% of the Hansatome group who attained this level of vision (see "Cumulative Uncorrected Visual Acuity, 1 Day OU"). The IntraLase group also had a slight edge at 20/20, with 93% seeing at this level vs. 86% of the Hansatome patients.
Measuring these eyes individually, we found that 19% of the IntraLase eyes had 20/15 vision vs. 8% of the Hansatome group (see "Cumulative Uncorrected Visual Acuity, 1 Day"). The IntraLase eyes also held an advantage at 20/20 (83% vs. 62%) and 20/25 (95% vs. 87%).

Measuring the eyes individually over the longer term, we found that significantly more IntraLase patients attained 20/15 vision (23% vs. 10%) compared with the Hansatome eyes (see "Cumulative Uncorrected Visual Acuity, up to 18 months postoperative"). The two groups basically evened out at 20/20 and below. Interestingly, the visual acuities at the longer-term follow-ups were not quite as good as those at 1-day.
Complications
Four of the 500 eyes (0.8%) treated with the Hansatome developed diffuse lamellar keratitis (DLK), while none of the IntraLase eyes encountered this complication. In fact, after more than 7,000 procedures using the IntraLase FS laser, not once have we had to lift a cap and irrigate it because of DLK.

We didn't study microstriae, but from my experience, I feel there are fewer microstriae with the IntraLase eyes than with the Hansatome eyes. If you look carefully at the Hansatome caps, you'll find that frequently the center is thin. That's not the case with the planar caps produced by the IntraLase unit, which are equally thick throughout. Because of that thickness in the center, fewer striae develop. But you still get striae to some extent in some eyes, especially in high myopes.
Precision flap architecture
I usually make 110-micron caps unless the patient is a high myope. In this case, I wish to conserve corneal tissue, so I'll make a 90- or 100-micron cap.
I measure some but not all caps and find that the thickest is about 140 microns (if I aim for 110). So I'm confident that our standard deviation is about 10 or 15 microns. Whereas with a metal keratome and a 160-micron head, you don't know whether you'll get 100 microns or 180 microns. That range is undesirable, especially if you're are working with a high myope.

The IntraLase femtosecond laser is a safe and effective alternative to the Hansatome microkeratome. Its attendant complications are relatively minor, and it allows for surgical flexibility in creating the flap architecture.
The 1-day post-op uncorrected visual acuities are very good in most patients. That's important, because good vision right from the start creates enthusiasm among patients, who are then more likely to recommend the procedure to family members and friends.
Dr. Manger practices at the Saddleback Eye Center in Laguna Hills, Calif.
SPONSORED BY

This is one of a series of articles recapping presentations given at the IntraLase booth during the 2003 meeting of the American Academy of Ophthalmology.








